Schizophrenia: An Overview
- Reviewed5 Jun 2023
- Author Alison Davis
- Source BrainFacts/SfN

While many psychiatric disorders impact a person’s behavior, mood, and cognition, most disorders don’t tend to significantly alter a person’s sensory reality. Schizophrenia, however, can bring on psychosis (e.g., hallucinations and delusions), flattened or blunted emotions, and impaired cognitive function.
Schizophrenia is a lifelong, severe psychiatric disorder that significantly alters thinking, emotion, and behavior. People with schizophrenia appear to others to have lost touch with reality. They experience “positive” symptoms such as hallucinations, delusions, and confused thinking, and “negative” ones, including an inability to experience pleasure and a severe lack of motivation. Like many psychiatric disorders that first emerge when the human brain matures in the late teens and early 20s, schizophrenia usually appears *between late teens to early 20s in males and early 20s to early 30s in females.
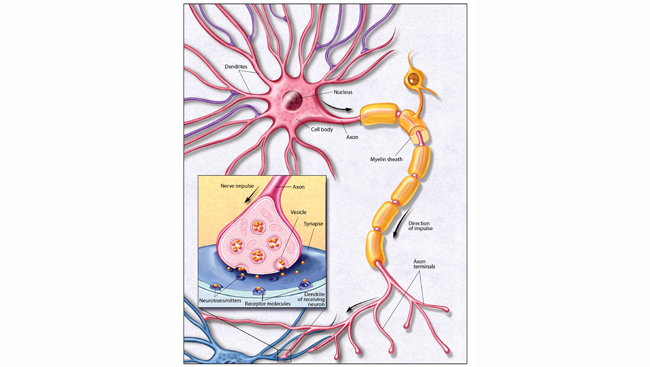
Although current medications do not provide a cure for schizophrenia, the combination of psychological treatments and medications provide the support needed for many people to pursue meaningful recovery goals. Chlorpromazine, the first antipsychotic drug, was developed in the 1950s as an anesthetic for surgery but was soon employed to calm people with psychiatric disorders including schizophrenia. Since then, more than 20 similar antipsychotic drugs have been developed. Most of these drugs work by dampening the dopamine response, which is thought to drive schizophrenia’s positive symptoms. For that reason, these medications may cause tremors and other movement-related side effects resembling Parkinson’s disease, which involves low dopamine activity. The most recently developed drugs also suppress some serotonergic activity, which seems to help with the negative symptoms of schizophrenia.
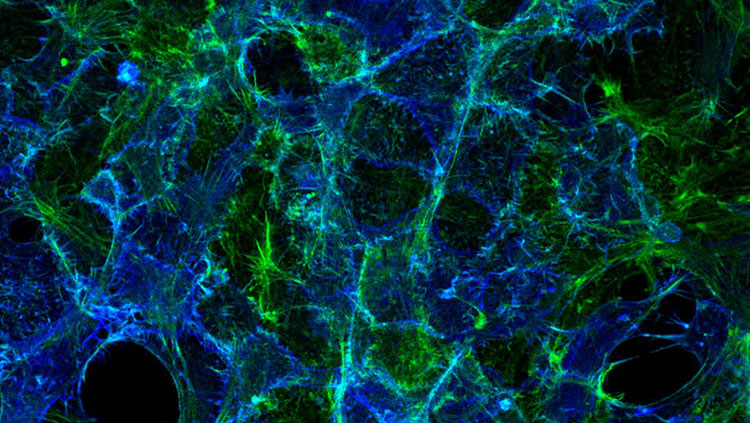
Scientists have known for many years, through studying twins and extended families with a history of schizophrenia, that this condition is highly influenced by heredity. With the emergence of powerful tools that scan massive amounts of DNA information, scientists in the last 15 to 20 years have been able to conduct hundreds of studies of gene association and risk for schizophrenia. Numerous genome-wide association studies have documented risk for schizophrenia typically involves many genes (more than 100) that each have a very small effect. Research continues to focus on learning more about genes that may impact schizophrenia, which affect nerve cell growth, development, learning, and memory. Genes with a proven relationship to schizophrenia are potential targets for new medications.
Adapted from the 8th edition of Brain Facts by Alison Davis.
*These age ranges were updated June 5, 2023, to reflect the most recent consensus from NIMH.
CONTENT PROVIDED BY
BrainFacts/SfN
References
Bandelow, B., & Michaelis, S. (2015). Epidemiology of anxiety disorders in the 21st century. Dialogues in Cclinical Nneuroscience, 17(3), 327–335. https://doi.org/10.31887/DCNS.2015.17.3/bbandelow
Burguière, E., Monteiro, P., Mallet, L., Feng, G., & Graybiel, A. M. (2015). Striatal circuits, habits, and implications for obsessive-compulsive disorder. Current Oopinion in Nneurobiology, 30, 59–65. https://doi.org/10.1016/j.conb.2014.08.008
Craddock, N., & Sklar, P. (2013). Genetics of bipolar disorder. Lancet (London, England), 381(9878), 1654–1662. https://doi.org/10.1016/S0140-6736(13)60855-7
Foland-Ross, L. C., Hamilton, P., Sacchet, M. D., Furman, D. J., Sherdell, L., & Gotlib, I. H. (2014). Activation of the medial prefrontal and posterior cingulate cortex during encoding of negative material predicts symptom worsening in major depression. Neuroreport, 25(5), 324–329. https://doi.org/10.1097/WNR.0000000000000095
Geddes, J. R., & Miklowitz, D. J. (2013). Treatment of bipolar disorder. Lancet (London, England), 381(9878), 1672–1682. https://doi.org/10.1016/S0140-6736(13)60857-0
Kavanagh, D. H., Tansey, K. E., O'Donovan, M. C., & Owen, M. J. (2015). Schizophrenia genetics: emerging themes for a complex disorder. Molecular Ppsychiatry, 20(1), 72–76. https://doi.org/10.1038/mp.2014.148
Memon, M. A. (2018). Panic Disorder. Medscape. http://emedicine.medscape.com/article/287913-overview
National Alliance on Mental Illness. (2017). Depression. https://www.nami.org/Learn-More/Mental-Health-Conditions/Depression
National Institute of Mental Health. (2017). Anxiety Disorders. NIH. https://www.nimh.nih.gov/health/topics/anxiety-disorders/index.shtml
National Institute of Mental Health. (2017). Bipolar Disorder. NIH. https://www.nimh.nih.gov/health/statistics/prevalence/bipolar-disorder-among-adults.shtml
National Institute of Mental Health. (2017). Depression. NIH. https://www.nimh.nih.gov/health/topics/depression/index.shtml
National Institute of Mental Health. (2017). Obsessive-Compulsive Disorder (OCD). NIH. https://www.nimh.nih.gov/health/topics/obsessive-compulsive-disorder-ocd/index.shtml
National Institute of Mental Health. (2017). Panic Disorder. NIH. https://www.nimh.nih.gov/health/statistics/prevalence/panic-disorder-among-adults.shtml
National Institute of Mental Health. (2017). Post-Traumatic Stress Disorder (PTSD). NIH. https://www.nimh.nih.gov/health/statistics/prevalence/post-traumatic-stress-disorder-among-adults.shtml
Pittenger, C., & Bloch, M. H. (2014). Pharmacological treatment of obsessive-compulsive disorder. The Psychiatric Cclinics of North America, 37(3), 375–391. https://doi.org/10.1016/j.psc.2014.05.006
Ragen, B. J., Seidel, J., Chollak, C., Pietrzak, R. H., & Neumeister, A. (2015). Investigational drugs under development for the treatment of PTSD. Expert Opinion on Investigational Drugs, 24(5), 659–672. https://doi.org/10.1517/13543784.2015.1020109
Strube, W., Bunse, T., Nitsche, M. A., Wobrock, T., Aborowa, R., Misewitsch, K., Herrmann, M., Falkai, P., & Hasan, A. (2015). Smoking restores impaired LTD-like plasticity in schizophrenia: a transcranial direct current stimulation study. Neuropsychopharmacology, 40(4), 822–830. https://doi.org/10.1038/npp.2014.275
Treadway, M. T., Waskom, M. L., Dillon, D. G., Holmes, A. J., Park, M. T. M., Chakravarty, M. M., Dutra, S. J., Polli, F. E., Iosifescu, D. V., Fava, M., Gabrieli, J. D. E., & Pizzagalli, D. A. (2015). Illness progression, recent stress, and morphometry of hippocampal subfields and medial prefrontal cortex in major depression. Biological Psychiatry, 77(3), 285–294. https://doi.org/10.1016/j.biopsych.2014.06.018
World Health Organization. (2022). Mental disorders. https://www.who.int/news-room/fact-sheets/detail/mental-disorders