The Body’s Pain Control System
- Published1 Apr 2012
- Reviewed1 Apr 2012
- Source BrainFacts/SfN
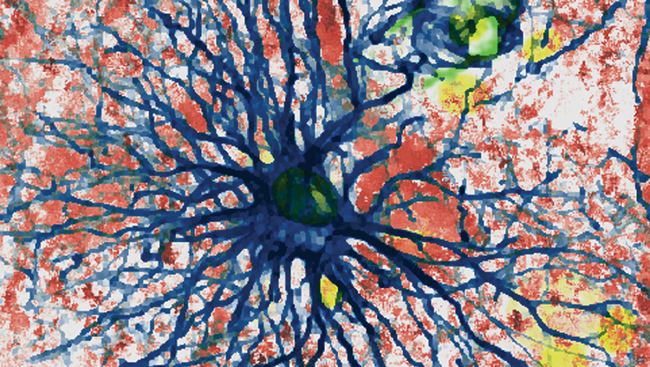
Studies of the body’s own pain-control system not only demonstrated the existence of naturally occurring opioids — the endorphins — but also identified the receptors through which opioids exert their effects.
The finding that opioid receptors are concentrated in the spinal cord led to the use of injections of morphine and other opioids into the cerebrospinal fluid in which the spinal cord is bathed, without causing paralysis, numbness, or other severe side effects. This technique came about through experiments with animals that first showed that injecting morphine into the spinal fluid could produce profound pain control. It is now commonly used in humans to treat pain after surgery, and to treat chronic pain in some patients by having them use an implanted pump.
New targets on the horizon
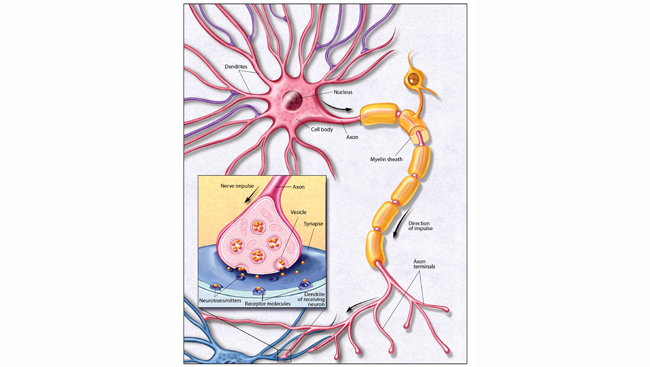
Molecular biology and genetic approaches have identified many molecules, such as ion channels and receptors, which are predominantly, if not exclusively, expressed by the nociceptor, the peripheral nerve fiber that initially responds to the injury stimulus. Because adverse side effects of drugs arise from the widespread location of the molecules targeted by analgesics — for example, constipation results from morphine’s action on opioid receptors in the gut — new analgesics that target only the nociceptor may have fewer side effects.
Among the many nociceptor targets are specialized receptor channels — one of which is activated by capsaicin, the pungent ingredient in hot peppers, and another by mustard oil — as well as a variety of acid-sensing sodium and calcium ion channels. Blocking the activity of many of these molecules has proven effective in animal studies, suggesting that the development of drugs that target these molecules in humans may have great value for the treatment of acute and persistent pain. Following from these findings, topical (skin) application of high doses of capsaicin has recently been approved for some neuropathic pain conditions. This treatment likely kills the sensing portion of pain fibers, but because these nerve fibers will regenerate, treatment needs to be repeated.
Pain is a complex experience that is largely a product of brain function. The pain is in the brain, not in the nociceptors that respond to the injury. Pain also involves emotional factors, so previous experiences with pain can have an impact on a more recent experience. All of these variables must be addressed concurrently in order to treat pain. The fact that placebos and hypnosis can significantly reduce pain clearly illustrates the importance of these psychological factors.
CONTENT PROVIDED BY
BrainFacts/SfN