Nicotine Addiction
- Published22 Mar 2009
- Reviewed22 Mar 2009
- Author Sarah Bates, MS, MA
- Source BrainFacts/SfN
New insight into nicotine and its effect on the brain helps researchers develop novel approaches to treating tobacco addiction.
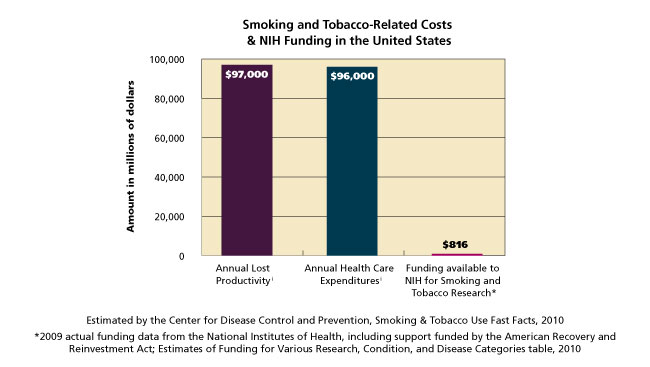
One in every five U.S. deaths each year is smoking-related. Yet, despite the health risks, more than 80 percent of smokers who try to quit fail within the first year, due to their chemical dependence. With support from national funding agencies such as the U.S. National Institutes of Health, and private and public partnerships, novel therapies born from basic research are fast becoming viable methods to help smokers quit for good.
Tools From Unlikely Places Lead to Big Advances in Nicotine Research
Although people have smoked or chewed tobacco for hundreds of years, exactly how nicotine affects the brain — making users feel more calm and alert — was not known until the 1970s.
Nicotine at Work in the Brain
After a person inhales cigarette smoke, nicotine molecules enter the blood stream and travel to the brain. But what does nicotine do after it arrives there? At the start of the 20th century, scientists reasoned that nicotine acted on some sort of "receptive substance" in the brain that received the chemical and transmitted it. While researchers realized such a receptor likely existed, they were unable to find it.
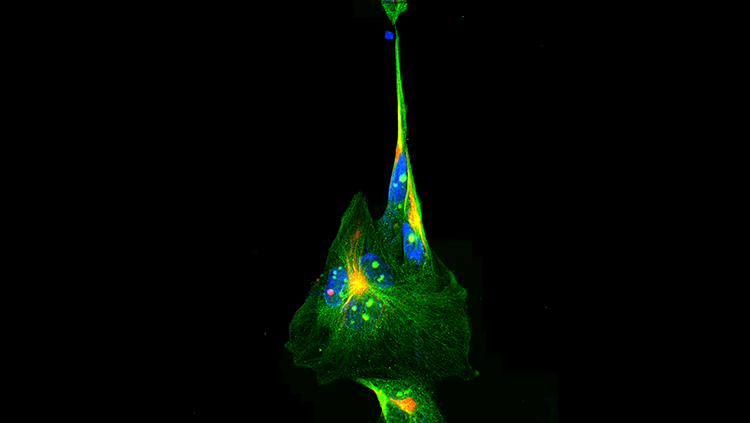
In the 1970s, researchers used some unusual materials to identify the receptor. They started with cells from an electric fish, an animal with a simple nervous system that could serve as a basic model. They then added a toxin from snake venom, which blocked the effects of nicotine. These results confirmed that a distinct protein picks up and relays signals from nicotine.
Finding this first receptor revolutionized neuroscience. Since this discovery, other receptors and neurotransmitters have been identified, allowing researchers a glimpse into the complexities of nerve cell communication. These particular receptors, called nicotinic acetylcholine receptors, are normally activated by the body's own acetylcholine, one of many chemical messengers that transmit information in the nervous system. Nicotine hijacks these receptors in the brain, taking over the role acetylcholine typically fills.
Locating the nicotine receptor was only the beginning. Scientists now study these receptors to learn about the chemical processes and behaviors associated with nicotine addiction.
A reward system held hostage by an addictive drug
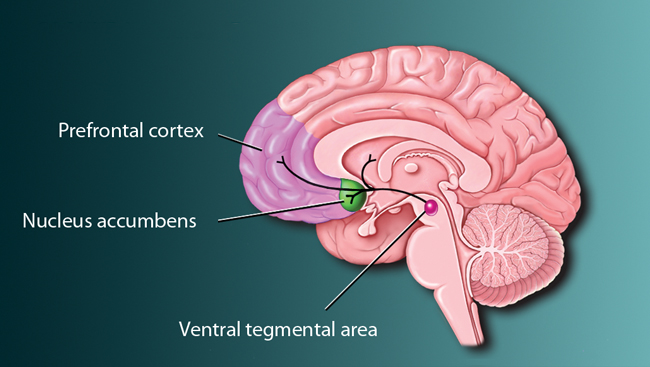
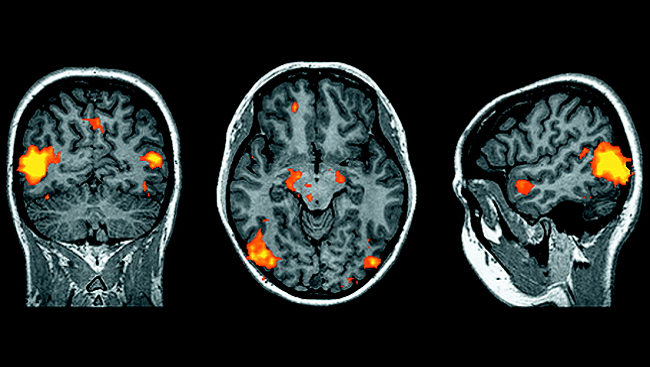
Nicotine, like cocaine and heroin, takes over the brain pathways that control pleasure. This "reward pathway" starts in the ventral tegmental area with cells that are covered with nicotine receptors and make the chemical dopamine. From there, these cells connect to the nucleus accumbens, which influences reward and pleasure, and the prefrontal cortex, which is associated with decision-making.
Feelings of enjoyment from the dopamine surge make users want to take more. Studies show that rats will self-administer electrical current directly into reward centers to receive such pleasure. However, the reward pathway eventually adapts to the foreign chemical, the brain becomes dependent, and the smoker ends up addicted.
Addiction Depends Partly on Genes
Scientists now know that addiction risk varies from person to person. Genetics, along with environment, help determine how far that first puff goes to get a smoker hooked.
How an individual responds to nicotine may depend on the makeup of their nicotinic acetylcholine receptors. A nicotinic receptor molecule contains five subunits, each generated from its own gene. Recent research shows that receptor subunit genes have a big affect on how animals — and likely humans — react to nicotine.
In an influential study, scientists genetically modified mice to make a receptor subunit called alpha-4 (α4) hypersensitive to nicotine. Triggering this single subunit with small amounts of nicotine made the mice more likely to show signs of addiction. Other researchers found that removing the gene associated with the beta-2 (β2) subunit made mice less vulnerable to addiction.
These findings suggest that the α4 and β2 subunits play important roles in addiction. Consistent with the animal research, studies show that human smokers have more of these subunits as a result of smoking. Having more of these subunits may make it especially hard to quit.
Additional addiction research indicates key roles of other subtypes. Large-scale studies aimed at spotting genetic risk factors are ongoing, with the goal of tailoring treatment options to people based on their biology.
Research opens up new treatment options
The most effective methods for stopping tobacco use ease withdrawal symptoms and block the pleasant effects of nicotine. Ideally, treatment also makes nicotine repulsive to further discourage the habit.
New Treatment in a Vaccine
One new remedy now in clinical trials is delivered in the form of a vaccine. The vaccine prompts a smoker's immune system to produce antibodies that attach to the nicotine molecules, preventing them from entering the brain. Without these chemical deliveries, nicotine would have no effect. It follows that there would be no reason to smoke.The nicotine vaccine was born from collaboration between the National Institute on Drug Abuse and private companies, highlighting the value of cooperation in future research.
Drugs used to treat other diseases also are being explored to find out how they affect smoking behavior. For instance, epilepsy drugs have been shown to block nicotine's effects. Genetic tests may help find which medications are best suited for an individual. Regardless of which type of treatment is followed, most experts believe behavioral therapy is still needed to teach ex-smokers how to cope with everyday stress and the temptation to relapse.
High Points and Hurdles of Quitting
People who quit smoking immediately lower their risk for cancers, heart disease, and stroke. According to the Centers for Disease Control and Prevention, a 35-year-old man who stops smoking increases his life expectancy by about five years.
Studies show most smokers want to stop. Smokers who use a nicotine patch, gum, or other cessation aid increase their odds of long-term success by two to three times, particularly if paired with behavioral therapy. Yet, even with today's treatments, only about 50 percent of smokers who enter an extended program are smoke-free a year later. New methods are clearly needed, and research is paving the way.
CONTENT PROVIDED BY
BrainFacts/SfN
Also In Archives
Trending
Popular articles on BrainFacts.org