Are Commercial Vagus Nerve Stimulation Devices Safe and Effective?
- Published24 Apr 2019
- Author Michael W. Richardson
- Source BrainFacts/SfN
The longest of the 12 cranial nerves, the vagus nerve meanders all the way from the brain to a host of body systems, including the heart, digestive system, and immune system. For this reason, it’s the site of potential treatments for various disorders and conditions connected to the brain and body. There are currently commercial devices on the market aimed at stimulating the nerve, though their effectiveness remains in question. Denise Bellinger, associate research professor at Loma Linda University, explains vagus nerve stimulation, the difference between clinical and commercial devices, and their safety and efficacy.
What is the vagus nerve?
The vagus nerve is an autonomic nerve that runs from the brain down through the body cavity. It has an excitatory side and an inhibitory side that work together as a yin-yang system to regulate the activities of multiple organ systems — the heart, GI system, immune system, and other organs throughout the body. The nerve’s connection to the heart allows the brain to regulate heart beats according to your environment and experiences. The vagus nerve slows down the heart. It counteracts the sympathetic nervous system. Similarly, the sympathetic nerves divert blood from the gastrointestinal tract skeletal muscles so that you can fight or take flight. The vagus nerve promotes digestion and restorative functions of the body.
How long has VNS been in use and what disorders could it treat?
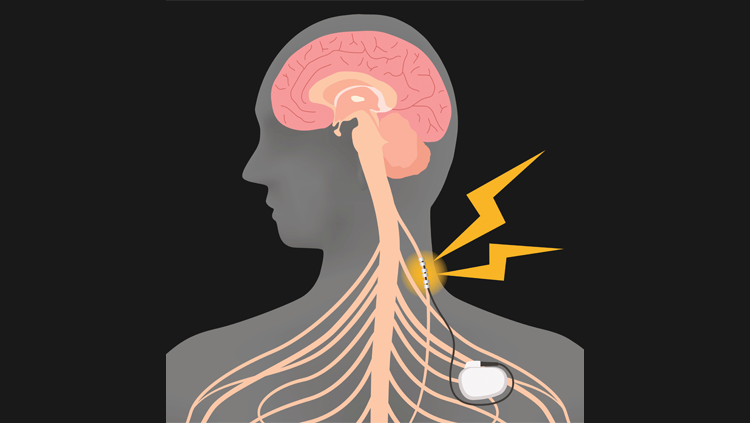
Vagus nerve stimulation (VNS) has been around since the 1990s. Doctors isolate the nerve — typically in the neck, where it’s most accessible — and surgically attach electrodes directly to the nerve to help promote a resting and body restorative state. Doctors must set it at a specific frequency, determine how often the electric signals will fire, and regulate the activity, even after the device is installed in the body.
VNS dampens sympathetic nerve activity that supplies many organs and where there is a dual sympathetic and vagal nerve. In this case, the vagus nerve exerts an opposing effect to the effects of the sympathetic nerves. There is also a sensory component of the vagus nerve that conveys information about the functioning and well-being of the visceral organs to the brain. The regions of the brain that receive this input are involved in regulating not only visceral organ functions, like the heart pumping blood to the body and how much oxygen is circulating through the blood vessels, but also modifying central autonomic and limbic systems. One benefit of VNS stimulation may be its activation of the afferent nerve fibers — those going to the brain. The afferent fibers can exert widespread effects on the autonomic, reticular, and limbic areas of the brain to affect mood, alertness and attention, and emotional responses to our experience.
VNS is effective at regulating and suppressing seizures associated with epilepsy — for patients who are unresponsive to medication, it can be a lifesaving device. It regularly pulses electricity to keep the brain in rhythm — like a how pacemaker works on the heart. Many patients with epilepsy experience an aura before the seizure begins, so some VNS devices allow the patient to initiate or increase the rate of VNS stimulation before the seizure can manifest. It’s also been floated as a treatment for many conditions, from depression to severe headaches. There aren’t many studies or trials on these treatments yet, but there seem to be promising signs.
How do external or commercial VNS devices differ from traditional clinical devices?
In addition to differences in frequencies and voltages, a fully external VNS device can’t obviously be implanted right on the nerve, like in clinical devices. External VNS devices rely on electrical signals that can pass through the skin and muscle of the neck while not affecting the tissue it’s passing through. It must still be precise enough to access and regulate specific activity of the nerve. Clinical VNS devices avoid exciting smaller fibers in the vagus nerve that convey pain; these are fibers you wouldn’t want to excite. However, larger fibers going into the brain are more likely the targeted site for potential treatments. Targeting these fibers is difficult for an external device that can’t be attached to specific nerve fibers.
Some VNS devices on the market are medical devices that require a doctor’s authorization. Others claim to be entertainment devices for relaxation. How should these devices be used, and what are the risks?
Commercial VNS devices have serious potential side effects like cardiac arrest because of this strong connection to the heart. Improper stimulation can cause problems with the cardiac system and trigger a heart attack. For that reason, VNS devices are generally applied only to the right side of the nerve because it has less direct connection to the heart.
We don’t know yet about long-term side effects. When you overstimulate nerves, they can release neurotransmitters that cause inflammation, both at the treatment site and further down the circuits. In older people, these nerves are more susceptible to damage from inflammation. While you’re treating symptoms at the central nervous system, you could be harming the peripheral nervous system. Like many medical interventions, it’s a balance between the treatment’s benefits and discomfort, and whether the latter can be tolerated.
Any patient researching VNS treatment should talk to a physician who specializes in this area. These devices should only be available through a prescription. A doctor who is familiar with the clinical trials and technology will have the correct expertise. I think these devices are brought to the clinical setting more rapidly than pharmaceuticals. The non-invasive devices are relatively new, but when used in the clinical setting they could reduce patient risk of potential complications due to surgical implantation of the device. I do not recommend the commercial VNS devices without doctor prescription and use monitoring. Internal devices remain the gold standard; non-invasive ones haven’t been fully proven yet to have the same fidelity.
I also think VNS devices could be a huge shift to treat these various conditions. All current medications come with side effects. If a device like this can improve your life and the way you function, it’s something worth researching and discussing with a doctor.
BrainFacts.org welcomes all your brain-related questions.
Every month, we choose one reader question and get an answer from a top neuroscientist. Always been curious about something?
Please submit your question by filling out this form.







