Pain can be acute — a short-lived warning sign of injury or disease — or a chronic condition that persists for months, or even years. For many people, pain is the disease itself.
*Chronic pain affects an estimated 50 million adults in the United States. Back, hip, knee, and foot pain are the most commonly reported culprits, with other frequent sources including pain from an old injury, infection, headaches, nerve damage, and diseases like cancer, arthritis, or diabetes. In the U.S., the cost of healthcare, disability, and lost productivity due to pain ranges from $560 billion to $635 billion annually. Chronic pain affects function and interferes with daily activities, sleep, work, and social interactions. Chronic pain can trigger a cascade of psychological processes that lead to changes in perception, attention, mood, motivation, learning, and memory. Increasing evidence points to the value of a combination of treatments involving drugs, and behavior and physical therapy, plus other modalities to fully manage chronic pain.
There are various types of pain. Nociceptive pain is caused by the activation of nociceptors at the site of injury. Neuropathic pain is caused by injury to the somatosensory system, or parts of the nervous system responsible for processing bodily touch and pain signals. Nociplastic pain may result from changes in central nervous system (CNS) processing, namely nociception processing, of pain. And chronic pain is caused, heightened, or prolonged by cognitive or behavioral factors.
Treating Pain
Physical therapy is usually the first line of treatment, aimed at applying non-drug treatments to improve function and reduce chronic pain. Physical therapy is a treatment that incorporates a variety of techniques, including teaching methods to manage pain (self-management), exercise, manual therapies like massage, and low-voltage electrical stimulation like transcutaneous electrical nerve stimulation (TENS). These non-drug treatments activate the body's own pain control mechanisms, including natural opioids. Regular exercise can help with chronic pain by working to reduce excitability of pain neurons, enhancing inhibition in the nervous system, changing the immune system to promote healing and reduce pain, and improving mood.
Psychological therapies such as cognitive behavioral therapy help people manage changes in mood, perception, memory, and other psychological factors often affected by chronic pain. Brain imaging studies have shown that psychological therapies alter brain circuitry in areas involved in processing pain and inhibition and help to change mood and maladaptive beliefs. Biofeedback can also be used to stimulate relaxation and release muscle tension, thereby helping reduce some of the effects of chronic pain.
Five main types of pain medications are typically used in clinical settings to relieve pain: nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin, ibuprofen, and naproxen; acetaminophen such as Tylenol; antiepileptic agents such as propofol and gabapentin; antidepressants such as amitriptyline; and opioids such as codeine, oxycodone, and hydromorphone.
NSAIDs, which reduce inflammation, are effective for acute pain and for pain caused by inflammation such as arthritis. NSAIDs are also useful for treating mild or moderate pain from headaches, sprains, toothaches, and back or neck pain. NSAIDs work by inhibiting substances that trigger the synthesis of pro-inflammatory and pain-producing chemicals (such as prostaglandins) across CNS and peripheral nervous systems. Moderate pain is often treated by combining a mild opioid like codeine with aspirin or another NSAID.
Acetaminophen is useful for treating mild to moderate pain from skin injuries, headaches, or conditions impacting the muscles and bones. Acetaminophen works similarly to NSAIDs; it is thought to block the production of pain-producing chemicals like prostaglandins. But acetaminophen does not target inflammation at the site of injury and primarily acts throughout the central nervous system. Acetaminophen is sometimes combined with an opioid to reduce the amount of opioid needed for pain treatment.
Antiepileptic and antidepressant drugs are generally used to treat nerve pain that results from enhanced central nervous system excitability or injury to the nervous system. Nerve damage and pain (neuropathy) can be due to chronic high blood sugar levels; viruses such as shingles; phantom limb pain; or post-stroke pain. Antiepileptic drugs directly modulate neuron activity by blocking channels involved in regulating activity of neurons, usually aimed at reducing excitation. Antidepressant drugs produce their effects by enhancing our endogenous inhibitory system through increasing neurotransmitters that reduce pain neuron activity (serotonin, noradrenaline). Both the antiepileptics and the antidepressants are given for neuropathic and nociplastic pain, or for pain with changes to central neuron excitability.
Opioids, often used for severe, acute pain, work directly in the central nervous system by attaching to opioid receptors. These drugs not only reduce pain but also produce feelings of euphoria. While effective against pain, opioids also have many serious side effects, such as slowing a person’s breathing. Most importantly, they are highly addictive. Opioids are currently the highest cause of prescription medication-related overdose deaths in the United States.
The Body’s Pain Control System
Studies of the body’s pain control system have shown that our bodies produce their own naturally occurring opioids, called endorphins. Scientists have also identified the receptors through which opioids work to decrease pain. Non-drug treatments like exercise and TENS work by increasing release of natural opioids to reduce pain, but do not have the side effects associated with taking an opioid medication.
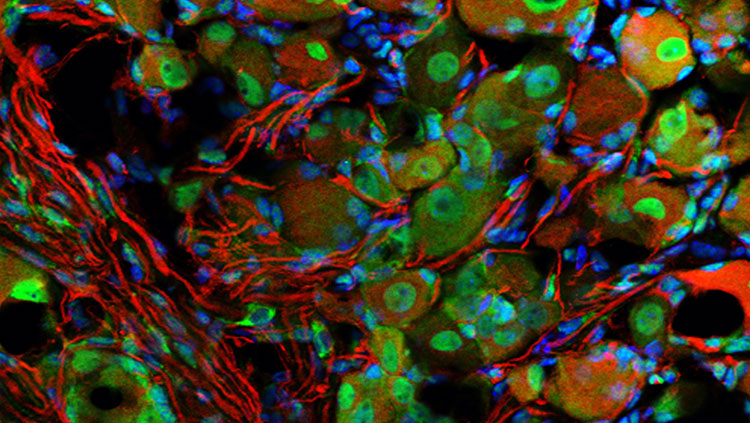
Scientists have identified many molecules that are involved in the body’s pain response. Developing drugs that target these molecules could have great benefit for treating patients who experience acute or chronic pain.
Advances in brain imaging techniques have also broadened our understanding of how the brain can prolong chronic pain even after a painful stimulus has been removed and injuries have healed. As a result, pain researchers are moving toward a whole-brain approach for their studies, developing new technologies and techniques that could lead to better diagnosis and more effective treatment of chronic pain.
*This paragraph was updated August 29, 2023 with the latest data on chronic pain prevalence and sources of chronic pain in the U.S. from the CDC’s National Health Interview Survey (NHIS).
Adapted from the 8th edition of Brain Facts by Gail Zyla.
CONTENT PROVIDED BY
BrainFacts/SfN
References
American Stroke Association. (2023). Types of Stroke and Treatment. https://www.stroke.org/en/about-stroke/types-of-stroke
Bang, O. Y., Kim, E. H., Cha, J. M., & Moon, G. J. (2016). Adult Stem Cell Therapy for Stroke: Challenges and Progress. Journal of stroke, 18(3), 256–266. https://doi.org/10.5853/jos.2016.01263
Centers for Disease Control and Prevention. (2017). HIV in the United States and Dependent Areas. https://web.archive.org/web/20230823143548/https://www.cdc.gov/hiv/statistics/overview/ataglance.html
Centers for Disease Control and Prevention. (2017). Stroke Facts. https://web.archive.org/web/20230820043558/https://www.cdc.gov/stroke/facts.htm
Centers for Disease Control and Prevention. (2017). Traumatic Brain Injury & Concussion. https://www.cdc.gov/TraumaticBrainInjury/
Chapman, S. N., Mehndiratta, P., Johansen, M. C., McMurry, T. L., Johnston, K. C., & Southerland, A. M. (2014). Current perspectives on the use of intravenous recombinant tissue plasminogen activator (tPA) for treatment of acute ischemic stroke. Vascular health and risk management, 10, 75–87. https://doi.org/10.2147/VHRM.S39213
Correale, J., Gaitán, M. I., Ysrraelit, M. C., & Fiol, M. P. (2017). Progressive multiple sclerosis: from pathogenic mechanisms to treatment. Brain : a journal of neurology, 140(3), 527–546. https://doi.org/10.1093/brain/aww258
Doulames, V. M., & Plant, G. W. (2016). Induced Pluripotent Stem Cell Therapies for Cervical Spinal Cord Injury. International journal of molecular sciences, 17(4), 530. https://doi.org/10.3390/ijms17040530
Gereau, R. W., 4th, Sluka, K. A., Maixner, W., Savage, S. R., Price, T. J., Murinson, B. B., Sullivan, M. D., & Fillingim, R. B. (2014). A pain research agenda for the 21st century. The journal of pain, 15(12), 1203–1214. https://doi.org/10.1016/j.jpain.2014.09.004
Krieger S. C. (2016). New Approaches to the Diagnosis, Clinical Course, and Goals of Therapy in Multiple Sclerosis and Related Disorders. Continuum (Minneapolis, Minn.), 22(3), 723–729. https://doi.org/10.1212/CON.0000000000000324
Martucci, K. T., Ng, P., & Mackey, S. (2014). Neuroimaging chronic pain: what have we learned and where are we going?. Future neurology, 9(6), 615–626. https://doi.org/10.2217/FNL.14.57
Matinella, A., Lanzafame, M., Bonometti, M. A., Gajofatto, A., Concia, E., Vento, S., Monaco, S., & Ferrari, S. (2015). Neurological complications of HIV infection in pre-HAART and HAART era: a retrospective study. Journal of neurology, 262(5), 1317–1327. https://doi.org/10.1007/s00415-015-7713-8
National Brain Tumor Society. (2023). Brain Tumor Facts. Brain Tumors. https://braintumor.org/brain-tumors/about-brain-tumors/brain-tumor-facts/
National Cancer Institute. (2017). Cancer Stat Facts: Brain and Other Nervous System Cancer. NIH. https://seer.cancer.gov/statfacts/html/brain.html
National Cancer Institute. (2023). Brain Tumor. NCI Dictionary of Cancer Terms. NIH. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/brain-tumor
National Spinal Cord Injury Statistical Center. (2017). University of Alabama at Birmingham. https://www.nscisc.uab.edu/
Okura, H., Smith, C. A., & Rutka, J. T. (2014). Gene therapy for malignant glioma. Molecular and cellular therapies, 2, 21. https://doi.org/10.1186/2052-8426-2-21
Reardon, D. A., Freeman, G., Wu, C., Chiocca, E. A., Wucherpfennig, K. W., Wen, P. Y., Fritsch, E. F., Curry, W. T., Jr, Sampson, J. H., & Dranoff, G. (2014). Immunotherapy advances for glioblastoma. Neuro-oncology, 16(11), 1441–1458. https://doi.org/10.1093/neuonc/nou212
Rosado, I. R., Lavor, M. S., Alves, E. G., Fukushima, F. B., Oliveira, K. M., Silva, C. M., Caldeira, F. M., Costa, P. M., & Melo, E. G. (2014). Effects of methylprednisolone, dantrolene, and their combination on experimental spinal cord injury. International journal of clinical and experimental pathology, 7(8), 4617–4626. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4152024/
Schonberg, D. L., Lubelski, D., Miller, T. E., & Rich, J. N. (2014). Brain tumor stem cells: Molecular characteristics and their impact on therapy. Molecular aspects of medicine, 39, 82–101. https://doi.org/10.1016/j.mam.2013.06.004
Schulenburg, A., Blatt, K., Cerny-Reiterer, S., Sadovnik, I., Herrmann, H., Marian, B., Grunt, T. W., Zielinski, C. C., & Valent, P. (2015). Cancer stem cells in basic science and in translational oncology: can we translate into clinical application?. Journal of hematology & oncology, 8, 16. https://doi.org/10.1186/s13045-015-0113-9
Simons, L. E., & Basch, M. C. (2016). State of the art in biobehavioral approaches to the management of chronic pain in childhood. Pain management, 6(1), 49–61. https://doi.org/10.2217/pmt.15.59
Simons, L. E., Elman, I., & Borsook, D. (2014). Psychological processing in chronic pain: a neural systems approach. Neuroscience and biobehavioral reviews, 39, 61–78. https://doi.org/10.1016/j.neubiorev.2013.12.006
Stuckey, D. W., & Shah, K. (2014). Stem cell-based therapies for cancer treatment: separating hope from hype. Nature reviews. Cancer, 14(10), 683–691. https://doi.org/10.1038/nrc3798
Su, Y. S., Ali, R., Feroze, A. H., Li, G., Lawton, M. T., & Choudhri, O. (2016). Endovascular therapies for malignant gliomas: Challenges and the future. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia, 26, 26–32. https://doi.org/10.1016/j.jocn.2015.10.019
Understanding the HIV Epidemic. (2017). Be in the KNOW. https://www.beintheknow.org/understanding-hiv-epidemic/data
Wang, S. X., Ho, E. L., Grill, M., Lee, E., Peterson, J., Robertson, K., Fuchs, D., Sinclair, E., Price, R. W., & Spudich, S. (2014). Peripheral neuropathy in primary HIV infection associates with systemic and central nervous system immune activation. Journal of acquired immune deficiency syndromes (1999), 66(3), 303–310. https://doi.org/10.1097/QAI.0000000000000167
White, H. & Venkatesh, B. (2016). Traumatic brain injury. Oxford Textbook of Neurocritical Care, 17. https://books.google.com/books?hl=en&lr=&id=o7hlCwAAQBAJ&oi=fnd&pg=PA210&dq=traumatic+brain+injury&ots=53PDiF2Jhx&sig=TPqEUTtTpGBJdRxBbZPcgO1pqpc#v=onepage&q=traumatic%20brain%20injury&f=false
What to Read Next
Also In Pain
Trending
Popular articles on BrainFacts.org