Understanding and Treating Brain Tumors
- Reviewed7 Aug 2023
- Author Gail Zyla
- Source BrainFacts/SfN
Each year, more than 94,000 people in the United States are likely to be diagnosed with a tumor that originates in their brain — a primary brain tumor.* An estimated 27,000 of these tumors will be malignant (cancerous), and 67,000 will be benign (noncancerous). In addition, up to 200,000 people will be diagnosed with brain tumors that develop when cancer cells from other parts of the body travel through the bloodstream to the brain. Called metastatic brain tumors, these cancers typically spread from tumors of the lung, breast, skin, colon, or kidney. Regardless of its origin, a tumor, or any space-occupying lesion in the brain, can be lethal — and thus surgical removal is required for survival.
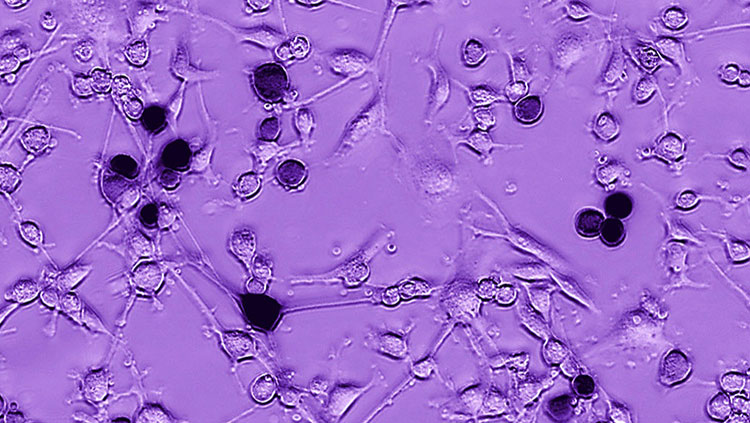
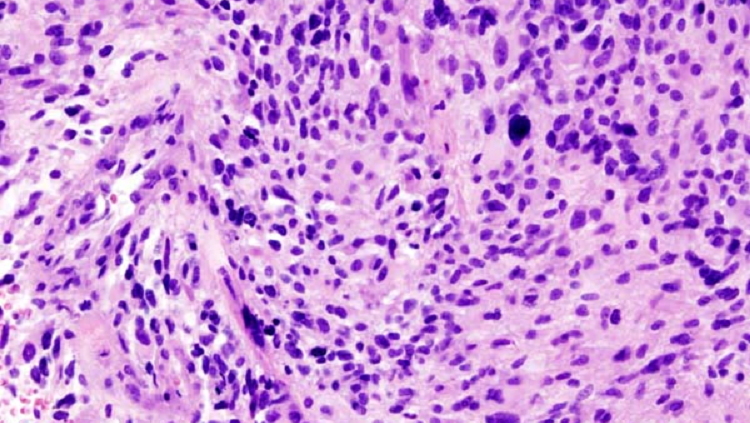
Types of brain tumors are named according to the kind of cell from which they arise and the brain area where they develop. For example, many brain tumors are called gliomas — a general term for tumors that arise from the glial cells that support and protect neurons in the brain. The most common form of brain cancer is glioblastoma — a proliferation of immature glial cells. The most common type of primary brain tumor is meningioma: a benign tumor arising in the meninges, thin layers of tissue that cover the brain.
Symptoms of a brain tumor depend on its location and size and vary among people. In some cases, a tumor causes general symptoms such as headaches, mainly due to the pressure a tumor exerts on the brain. Or a tumor located in a part of the brain controlling vision can cause difficulties with sight. In other cases, a tumor can damage healthy tissue as it grows. For example, as gliomas grow, they release toxic amounts of glutamate, which can destroy nerve cells near the tumor and cause seizures.
Several treatments — including surgery, radiation, targeted treatments, and chemotherapy — can be used alone or in combination to treat brain tumors. The goal of the treatments is to remove or shrink brain tumors to relieve pressure on the brain, as well as eliminating or reducing symptoms such as seizures and headaches.
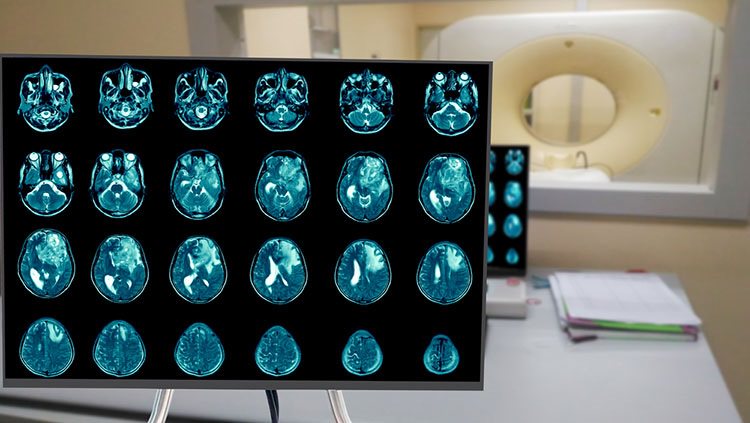
Neurosurgery is usually the first option to treat a brain tumor. Brain tumors can be removed with conventional techniques such as a craniotomy, in which the skull is opened and as much of the tumor as possible is removed. The extent to which a surgeon can perform a gross total resection (cutting out over 95% of the mass) is determined in part by proximity to eloquent brain areas involved in language, memory, and motor functions. Another type of treatment for some tumors uses radiation. For this technique, called stereotactic radiosurgery, a high dose of radiation is aimed precisely at the tumor. A few radiation treatments can reduce or eliminate the tumor while sparing healthy tissue nearby. More recently, tumors are treated by multiple beams of ultrasound focused precisely at the tumor site. These interventions can be carried out painlessly in conscious patients inside imaging machines that visualize the tumor in the brain.
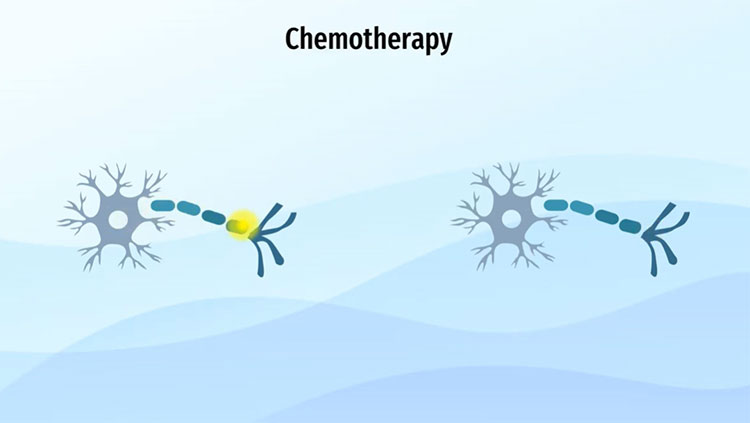
Following conventional surgery, doctors usually prescribe steroid medications to reduce swelling in the brain. Reduced swelling helps alleviate symptoms such as seizures, memory problems, or confusion that can occur after brain surgery. In patients with cancerous brain tumors, radiation may be administered to surrounding brain areas to help eliminate any cancer cells that remain in the brain after surgery. People with cancerous brain tumors can also be given chemotherapy to prevent growth or regrowth of their tumors. Researchers have developed new ways to administer chemotherapy that allow medication to be delivered directly to the brain (tumor), rather than traveling through the body before reaching the brain. For example, after surgical removal of a brain tumor, small wafers containing anticancer drugs can be implanted in the space previously occupied by the tumor. Over time, the wafers slowly dissolve and release the chemotherapy drugs to nearby areas.
Researchers have also been studying various promising treatments that target specific cell mechanisms thought to be important to cancer cell growth. These targeted treatments zero in on genes and other cell mechanisms that fuel cancer cell growth, while sparing healthy tissues and causing less severe side effects than those that occur with conventional radiation or chemotherapy. For example, medications that help block the formation of blood vessels are already being used to treat glioblastomas. Blocking tumor blood vessel formation is a key strategy in treating glioblastomas, because these tumors form strong networks of vessels that feed tumor growth.
Researchers are also testing ways to stimulate the ability of the body’s own immune system to stop tumor growth — an approach called immunotherapy. For example, promising research is using substances called checkpoint inhibitors, which interfere with the signals some tumors send to inhibit the immune system’s ability to block tumor growth.
Another promising area of research involves gene therapy. This technology identifies genetic components that promote tumor growth and then interferes with their ability to function. Research is currently underway on numerous different gene therapies aimed at killing tumor cells and suppressing their growth-promoting genes.
Other approaches also under development focus on targeted delivery of antibodies, toxins, and growth-inhibiting molecules that can attach specifically to tumor cells and interfere with their growth. Researchers are also exploring the role of stem cells in both the development and treatment of brain tumors. Stem cells are undifferentiated, or unspecialized, cells with the potential to develop into a number of specialized cells, such as neurons. Normally, regulatory processes prevent mature, specialized cells from dividing and spreading; cancer cells, however, escape these regulations. Investigating the normal processes that allow stem cells to mature will allow researchers to understand what might be going awry in cancer cells.
Adapted from the 8th edition of Brain Facts by Gail Zyla.
*The statistics on brain tumor prevalence were updated August 7, 2023 to reflect the most recent Central Brain Tumor Registry of the United States (CBTRUS) data on brain tumor prevalence in the U.S.
CONTENT PROVIDED BY
BrainFacts/SfN
References
Bang, O. Y., Kim, E. H., Cha, J. M., & Moon, G. J. (2016). Adult Stem Cell Therapy for Stroke: Challenges and Progress. Journal of stroke, 18(3), 256–266. https://doi.org/10.5853/jos.2016.01263
Centers for Disease Control and Prevention. (2017). HIV in the United States and Dependent Areas. https://web.archive.org/web/20230823143548/https://www.cdc.gov/hiv/statistics/overview/ataglance.html
Centers for Disease Control and Prevention. (2017). Stroke Facts. https://web.archive.org/web/20230820043558/https://www.cdc.gov/stroke/facts.htm
Centers for Disease Control and Prevention. (2017). Traumatic Brain Injury & Concussion. https://www.cdc.gov/TraumaticBrainInjury/
Chapman, S. N., Mehndiratta, P., Johansen, M. C., McMurry, T. L., Johnston, K. C., & Southerland, A. M. (2014). Current perspectives on the use of intravenous recombinant tissue plasminogen activator (tPA) for treatment of acute ischemic stroke. Vascular health and risk management, 10, 75–87. https://doi.org/10.2147/VHRM.S39213
Correale, J., Gaitán, M. I., Ysrraelit, M. C., & Fiol, M. P. (2017). Progressive multiple sclerosis: from pathogenic mechanisms to treatment. Brain : a journal of neurology, 140(3), 527–546. https://doi.org/10.1093/brain/aww258
Doulames, V. M., & Plant, G. W. (2016). Induced Pluripotent Stem Cell Therapies for Cervical Spinal Cord Injury. International journal of molecular sciences, 17(4), 530. https://doi.org/10.3390/ijms17040530
Gereau, R. W., 4th, Sluka, K. A., Maixner, W., Savage, S. R., Price, T. J., Murinson, B. B., Sullivan, M. D., & Fillingim, R. B. (2014). A pain research agenda for the 21st century. The journal of pain, 15(12), 1203–1214. https://doi.org/10.1016/j.jpain.2014.09.004
Krieger S. C. (2016). New Approaches to the Diagnosis, Clinical Course, and Goals of Therapy in Multiple Sclerosis and Related Disorders. Continuum (Minneapolis, Minn.), 22(3), 723–729. https://doi.org/10.1212/CON.0000000000000324
Martucci, K. T., Ng, P., & Mackey, S. (2014). Neuroimaging chronic pain: what have we learned and where are we going?. Future neurology, 9(6), 615–626. https://doi.org/10.2217/FNL.14.57
Matinella, A., Lanzafame, M., Bonometti, M. A., Gajofatto, A., Concia, E., Vento, S., Monaco, S., & Ferrari, S. (2015). Neurological complications of HIV infection in pre-HAART and HAART era: a retrospective study. Journal of neurology, 262(5), 1317–1327. https://doi.org/10.1007/s00415-015-7713-8
National Brain Tumor Society. (2023). Brain Tumor Facts. Brain Tumors. https://braintumor.org/brain-tumors/about-brain-tumors/brain-tumor-facts/
National Cancer Institute. (2017). Cancer Stat Facts: Brain and Other Nervous System Cancer. NIH. https://seer.cancer.gov/statfacts/html/brain.html
National Cancer Institute. (2023). Brain Tumor. NCI Dictionary of Cancer Terms. NIH. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/brain-tumor
National Spinal Cord Injury Statistical Center. (2017). University of Alabama at Birmingham. https://www.nscisc.uab.edu/
Okura, H., Smith, C. A., & Rutka, J. T. (2014). Gene therapy for malignant glioma. Molecular and cellular therapies, 2, 21. https://doi.org/10.1186/2052-8426-2-21
Reardon, D. A., Freeman, G., Wu, C., Chiocca, E. A., Wucherpfennig, K. W., Wen, P. Y., Fritsch, E. F., Curry, W. T., Jr, Sampson, J. H., & Dranoff, G. (2014). Immunotherapy advances for glioblastoma. Neuro-oncology, 16(11), 1441–1458. https://doi.org/10.1093/neuonc/nou212
Rosado, I. R., Lavor, M. S., Alves, E. G., Fukushima, F. B., Oliveira, K. M., Silva, C. M., Caldeira, F. M., Costa, P. M., & Melo, E. G. (2014). Effects of methylprednisolone, dantrolene, and their combination on experimental spinal cord injury. International journal of clinical and experimental pathology, 7(8), 4617–4626. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4152024/
Schonberg, D. L., Lubelski, D., Miller, T. E., & Rich, J. N. (2014). Brain tumor stem cells: Molecular characteristics and their impact on therapy. Molecular aspects of medicine, 39, 82–101. https://doi.org/10.1016/j.mam.2013.06.004
Schulenburg, A., Blatt, K., Cerny-Reiterer, S., Sadovnik, I., Herrmann, H., Marian, B., Grunt, T. W., Zielinski, C. C., & Valent, P. (2015). Cancer stem cells in basic science and in translational oncology: can we translate into clinical application?. Journal of hematology & oncology, 8, 16. https://doi.org/10.1186/s13045-015-0113-9
Simons, L. E., & Basch, M. C. (2016). State of the art in biobehavioral approaches to the management of chronic pain in childhood. Pain management, 6(1), 49–61. https://doi.org/10.2217/pmt.15.59
Simons, L. E., Elman, I., & Borsook, D. (2014). Psychological processing in chronic pain: a neural systems approach. Neuroscience and biobehavioral reviews, 39, 61–78. https://doi.org/10.1016/j.neubiorev.2013.12.006
Stuckey, D. W., & Shah, K. (2014). Stem cell-based therapies for cancer treatment: separating hope from hype. Nature reviews. Cancer, 14(10), 683–691. https://doi.org/10.1038/nrc3798
Su, Y. S., Ali, R., Feroze, A. H., Li, G., Lawton, M. T., & Choudhri, O. (2016). Endovascular therapies for malignant gliomas: Challenges and the future. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia, 26, 26–32. https://doi.org/10.1016/j.jocn.2015.10.019
Understanding the HIV Epidemic. (2017). Be in the KNOW. https://www.beintheknow.org/understanding-hiv-epidemic/data
Wang, S. X., Ho, E. L., Grill, M., Lee, E., Peterson, J., Robertson, K., Fuchs, D., Sinclair, E., Price, R. W., & Spudich, S. (2014). Peripheral neuropathy in primary HIV infection associates with systemic and central nervous system immune activation. Journal of acquired immune deficiency syndromes (1999), 66(3), 303–310. https://doi.org/10.1097/QAI.0000000000000167
White, H. & Venkatesh, B. (2016). Traumatic brain injury. Oxford Textbook of Neurocritical Care, 17. https://books.google.com/books?hl=en&lr=&id=o7hlCwAAQBAJ&oi=fnd&pg=PA210&dq=traumatic+brain+injury&ots=53PDiF2Jhx&sig=TPqEUTtTpGBJdRxBbZPcgO1pqpc#v=onepage&q=traumatic%20brain%20injury&f=false
What to Read Next
Also In Cancer
Trending
Popular articles on BrainFacts.org