How COVID-19 Attacks the Brain and Nervous System
- Published5 Nov 2021
- Author Alexis Wnuk
- Source BrainFacts/SfN
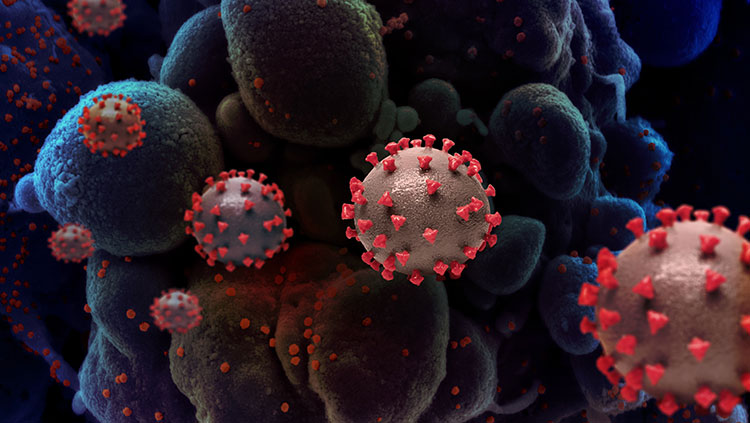
New research suggests SARS-CoV-2, the virus that causes COVID-19, can infect neurons and disrupt brain signaling for months post-infection. While the findings are preliminary — they have yet to be peer-reviewed or published in a journal — the research yields further insight into how the virus affects the nervous system and hints at possible therapeutic targets to mitigate these effects. Researchers presented their work at press conference held in association with the annual conference of the Society for Neuroscience on November 2.
Studying rhesus monkeys, researchers at the California National Primate Research Center found evidence of infection in the brain’s neurons. After infecting monkeys with the SARS-CoV-2 virus, the team examined their brains seven days post-infection, staining brain tissue with fluorescent molecules that tagged viral proteins and genetic material. They found the virus in the olfactory tubercle, a region of the cortex that receives signals from the olfactory bulbs. More surprisingly, they also found viral proteins in the entorhinal cortex, a swath of tissue involved in memory, navigation, and time perception.
“That’s your key link to Alzheimer’s,” John Morrison, director of the California National Primate Research Center and author of the study, said at a press briefing. “The entorhinal cortex is the single most vulnerable brain region to Alzheimer’s disease.”
A separate team of researchers found the virus can also infect nerves outside of the brain. Jonathan Joyce and collaborators at Virginia Tech infected mice with the virus. Three and six days later, they spotted the virus in structures called ganglia, collections of neuron cell bodies that relay information to and from the nervous system.
How the virus enters these neurons is an open question. “All of these ganglia have nerve endings out there in the periphery that are wide open for interaction between the virus and the nervous system,” said Joyce, a third-year PhD student. “But what mediates that has yet to be determined.”
A study by Ashutosh Kumar and colleagues at the All India Institute of Medical Sciences may offer a few clues. His team was inspired by work from other researchers published earlier this year, which identified an alternative entry point for the virus to enter cells: the neuropilin 1 receptor and an enzyme called furin.
By analyzing databases of gene and protein expression in the human brain, they found these proteins were widely expressed throughout the brain. In contrast, the ACE2 receptor— the protein granting the virus entry into lung cells — was barely detectible. “Our study unravels potential mediators for SARS-CoV-2 entry in [the] human brain,” Kumar said.
It’s unknown how long the virus might hang around in the brain and nervous system. But, the experiences of people with “long COVID” — who report pain, memory lapses, fatigue, and brain fog — suggest the effects can linger for months. A study of brain activity patterns bears this out. Researchers at the Rotman Research Institute in Toronto found COVID-19 diminishes brainpower for a least seven months after infection.
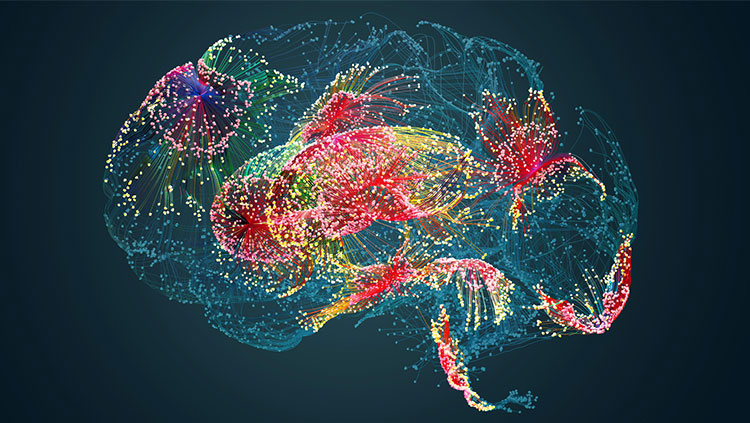
Allison Sekuler and her colleagues outfitted volunteers with portable electroencephalography (EEG) scanners to measure their brain’s electrical activity. In particular, they were interested in the power of the EEG signal, a measure of “the strength or coordination of brain signals,” Sekuler said. People who tested positive for COVID-19 had weaker EEG power than people with COVID-like symptoms who tested negative for the virus. What’s more, “the power remained lower for people who had been infected with COVID even after seven months,” Sekuler said.
When loss of sense of smell was first reported as a symptom of COVID-19, it suggested the virus might attack the nervous system. But whether the virus invaded neurons or affected them via a less direct route — like systemic inflammation or damage to support cells — has been a subject of debate.
The evidence presented on Tuesday likely won’t settle it. “I think that’s still pretty controversial,” Walter Koroshetz, director of the National Institute of Neurological Disorders and Stroke, said at a press briefing on November 3. “As an NIH director, I would probably punt and say we’ll have to see how the evidence comes out in the end. The good news is that if it is happening, it’s not rampant.”
CONTENT PROVIDED BY
BrainFacts/SfN
Also In COVID-19
Trending
Popular articles on BrainFacts.org