Sometimes before a video begins to play, a message reads, “Warning: This video may potentially contain seizure triggers for those with photosensitive epilepsy.” Heeding this warning can help prevent seizures, or sudden, uncontrolled bursts of electrical activity in the brain, for people with certain types of epilepsy.
Epilepsy affects about 50 million people worldwide. People who have two or more seizures that cannot be explained by a temporary underlying medical condition, such as a high fever or low blood sugar, will receive a medical diagnosis of “epilepsy” — from the Greek word epilambanein, meaning “to be seized.”
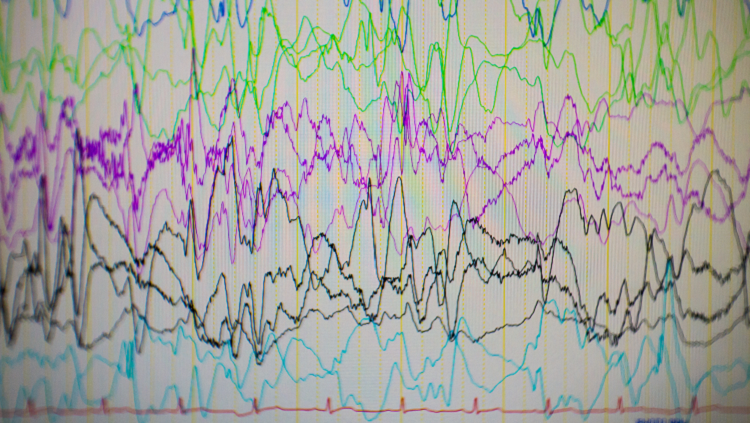
Seizures result from irregular activities in brain cells lasting as long as five or more minutes at a time. Some seizures look like staring spells, while others cause people to collapse, shake, and become unaware of what is going on around them. The pattern of symptoms and after-seizure brain recordings using electroencephalograms (EEGs) are used to distinguish between different types of epilepsy and determine whether the true cause of the seizures is epilepsy or a different medical condition.
Seizures are classified by where they occur in the brain. Generalized seizures affect both sides of the brain. They include absence or petit mal seizures, which can cause rapid blinking or a few seconds of staring into space, and tonic-clonic or grand mal seizures, which can make someone fall, have muscle spasms, cry out, and/or lose consciousness. Focal or partial seizures are localized to one area of the brain. A simple focal seizure can cause twitching or a change in sensation, triggering strange smells or tastes. Complex focal seizures can leave a person confused and unable to answer questions or follow directions. A person can also have what’s known as secondary generalized seizures, which begin in one part of the brain but spread to become generalized seizures. In some patients with severe epilepsy, multiple types of seizure can occur at the same time.
Epilepsy has many possible causes and is thus considered a spectrum rather than a single disorder. Causes include premature birth, brain trauma, and abnormal development due to genetic factors. Attributes of epilepsy patients such as head size, movement disorders, and family history suggest that genetics is involved.
Seizures can also accompany or cause intellectual or psychiatric problems. For example, some seizures may suppress the growth of dendrites, leaving the person emotionally unsettled or less able to learn.
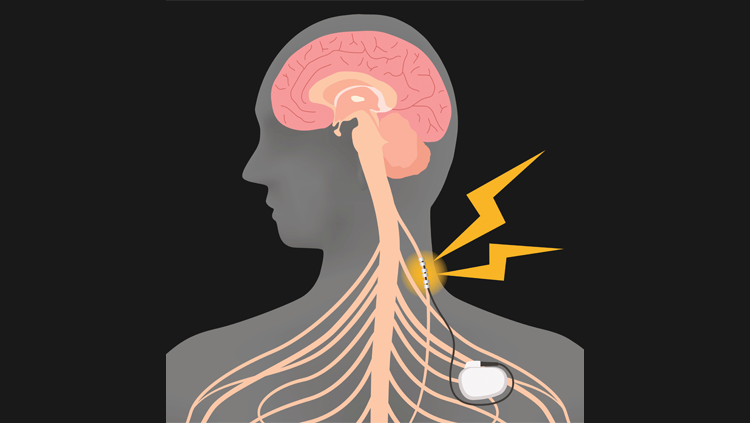
Treatments for epilepsy are directed toward controlling seizures with medication and/or diet. For most patients, a single medication is enough to control seizures, although a significant minority do not achieve adequate control from drugs. About half of epilepsy patients, particularly those with generalized epilepsy, can reduce their seizures by eating a ketogenic diet, which relies heavily on high-fat, low-carbohydrate foods, although it is unclear why this diet is effective. For severe cases that are not relieved by medication, doctors might recommend surgery to remove or inactivate the seizure-initiating part of the brain. In the most severe cases, if one side of the brain triggers seizures on the other side, surgeons may perform “split-brain surgery,” cutting the corpus callosum, a thick band of white matter that connects the two sides of the brain. Once their seizures are controlled, people with epilepsy can resume their normal lives.
Adapted from the 8th edition of Brain Facts by Karen Weintraub.
CONTENT PROVIDED BY
BrainFacts/SfN
References
Allen, E. G., Freeman, S. B., Druschel, C., Hobbs, C. A., O'Leary, L. A., Romitti, P. A., Royle, M. H., Torfs, C. P., & Sherman, S. L. (2009). Maternal age and risk for trisomy 21 assessed by the origin of chromosome nondisjunction: a report from the Atlanta and National Down Syndrome Projects. Human genetics, 125(1), 41–52. https://doi.org/10.1007/s00439-008-0603-8
Barbaresi, W. J., Colligan, R. C., Weaver, A. L., Voigt, R. G., Killian, J. M., & Katusic, S. K. (2013). Mortality, ADHD, and psychosocial adversity in adults with childhood ADHD: a prospective study. Pediatrics, 131(4), 637–644. https://doi.org/10.1542/peds.2012-2354
Bishop D. V. (2015). The interface between genetics and psychology: lessons from developmental dyslexia. Proceedings. Biological sciences, 282(1806), 20143139. https://doi.org/10.1098/rspb.2014.3139
Casanova, J. R., Nishimura, M., & Swann, J. W. (2014). The effects of early-life seizures on hippocampal dendrite development and later-life learning and memory. Brain research bulletin, 103, 39–48. https://doi.org/10.1016/j.brainresbull.2013.10.004
Casanova, M. (2015). The Neuropathology of Autism. In: Fatemi, S. (eds) The Molecular Basis of Autism. Contemporary Clinical Neuroscience. Springer, New York, NY. 153-171. https://doi.org/10.1007/978-1-4939-2190-4_8
Christensen, D. L., Baio, J., Braun, K. V., Bilder, D., Charles, J., Constantino, J. N., Daniels, J., Maureen, S. Durkin, M. S., Robert, T., Fitzgerald, R. T., Kurzius-Spencer, M., Lee, L., Pettygrove, S., Robinson, C., Schulz, E., Wells, C., Wingate, M. S., Zahorodny, W., Yeargin-Allsopp, M. (2016). Prevalence and Characteristics of Autism Spectrum Disorder Among Children Aged 8 Years — Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2012. MMWR Surveill Summ 2016;65(No. SS-3)(No. SS-3):1–23. DOI: http://dx.doi.org/10.15585/mmwr.ss6503a1external icon.
Chronis-Tuscano, A., Molina, B. S., Pelham, W. E., Applegate, B., Dahlke, A., Overmyer, M., & Lahey, B. B. (2010). Very early predictors of adolescent depression and suicide attempts in children with attention-deficit/hyperactivity disorder. Archives of general psychiatry, 67(10), 1044–1051. https://doi.org/10.1001/archgenpsychiatry.2010.127
Durkin, M. S., Maenner, M. J., Newschaffer, C. J., Lee, L. C., Cunniff, C. M., Daniels, J. L., Kirby, R. S., Leavitt, L., Miller, L., Zahorodny, W., & Schieve, L. A. (2008). Advanced parental age and the risk of autism spectrum disorder. American journal of epidemiology, 168(11), 1268–1276. https://doi.org/10.1093/aje/kwn250
Emerson, R. W., Adams, C., Nishino, T., Hazlett, H. C., Wolff, J. J., Zwaigenbaum, L., Constantino, J. N., Shen, M. D., Swanson, M. R., Elison, J. T., Kandala, S., Estes, A. M., Botteron, K. N., Collins, L., Dager, S. R., Evans, A. C., Gerig, G., Gu, H., McKinstry, R. C., Paterson, S., … Piven, J. (2017). Functional neuroimaging of high-risk 6-month-old infants predicts a diagnosis of autism at 24 months of age. Science translational medicine, 9(393), eaag2882. https://doi.org/10.1126/scitranslmed.aag2882
Finn, E. S., Shen, X., Holahan, J. M., Scheinost, D., Lacadie, C., Papademetris, X., Shaywitz, S. E., Shaywitz, B. A., & Constable, R. T. (2014). Disruption of functional networks in dyslexia: a whole-brain, data-driven analysis of connectivity. Biological psychiatry, 76(5), 397–404. https://doi.org/10.1016/j.biopsych.2013.08.031
Fisch, H., Hyun, G., Golden, R., Hensle, T. W., Olsson, C. A., & Liberson, G. L. (2003). The influence of paternal age on down syndrome. The Journal of urology, 169(6), 2275–2278. https://doi.org/10.1097/01.ju.0000067958.36077.d8
Frazier, T. W., Klingemier, E. W., Beukemann, M., Speer, L., Markowitz, L., Parikh, S., Wexberg, S., Giuliano, K., Schulte, E., Delahunty, C., Ahuja, V., Eng, C., Manos, M. J., Hardan, A. Y., Youngstrom, E. A., & Strauss, M. S. (2016). Development of an Objective Autism Risk Index Using Remote Eye Tracking. Journal of the American Academy of Child and Adolescent Psychiatry, 55(4), 301–309. https://doi.org/10.1016/j.jaac.2016.01.011
Geschwind, D. H., & State, M. W. (2015). Gene hunting in autism spectrum disorder: on the path to precision medicine. The Lancet. Neurology, 14(11), 1109–1120. https://doi.org/10.1016/S1474-4422(15)00044-7
Guastella, A. J., & Hickie, I. B. (2016). Oxytocin Treatment, Circuitry, and Autism: A Critical Review of the Literature Placing Oxytocin Into the Autism Context. Biological psychiatry, 79(3), 234–242. https://doi.org/10.1016/j.biopsych.2015.06.028
Hallmayer, J., Cleveland, S., Torres, A., et al. Genetic Heritability and Shared Environmental Factors Among Twin Pairs With Autism. Arch Gen Psychiatry. 2011;68(11):1095–1102. doi:10.1001/archgenpsychiatry.2011.76
Helguera, P., Seiglie, J., Rodriguez, J., Hanna, M., Helguera, G., & Busciglio, J. (2013). Adaptive downregulation of mitochondrial function in down syndrome. Cell metabolism, 17(1), 132–140. https://doi.org/10.1016/j.cmet.2012.12.005
Hornig, M., Bresnahan, M. A., Che, X., Schultz, A. F., Ukaigwe, J. E., Eddy, M. L., Hirtz, D., Gunnes, N., Lie, K. K., Magnus, P., Mjaaland, S., Reichborn-Kjennerud, T., Schjølberg, S., Øyen, A. S., Levin, B., Susser, E. S., Stoltenberg, C., & Lipkin, W. I. (2018). Prenatal fever and autism risk. Molecular psychiatry, 23(3), 759–766. https://doi.org/10.1038/mp.2017.119
Jiang, J., Jing, Y., Cost, G. J., Chiang, J. C., Kolpa, H. J., Cotton, A. M., Carone, D. M., Carone, B. R., Shivak, D. A., Guschin, D. Y., Pearl, J. R., Rebar, E. J., Byron, M., Gregory, P. D., Brown, C. J., Urnov, F. D., Hall, L. L., & Lawrence, J. B. (2013). Translating dosage compensation to trisomy 21. Nature, 500(7462), 296–300. https://doi.org/10.1038/nature12394
Kasparek, T., Theiner, P., & Filova, A. (2015). Neurobiology of ADHD From Childhood to Adulthood: Findings of Imaging Methods. Journal of attention disorders, 19(11), 931–943. https://doi.org/10.1177/1087054713505322
Katsnelson, A., Buzsáki, G., & Swann, J. W. (2014). Catastrophic childhood epilepsy: a recent convergence of basic and clinical neuroscience. Science translational medicine, 6(262), 262ps13.
Kozlowski, A. M., Matson, J. L., Horovitz, M., Worley, J. A., & Neal, D. (2011). Parents' first concerns of their child's development in toddlers with autism spectrum disorders. Developmental neurorehabilitation, 14(2), 72–78. https://doi.org/10.3109/17518423.2010.539193
Lainhart J. E. (2015). Brain imaging research in autism spectrum disorders: in search of neuropathology and health across the lifespan. Current opinion in psychiatry, 28(2), 76–82. https://doi.org/10.1097/YCO.0000000000000130
Lord, C., Risi, S., DiLavore, P. S., Shulman, C., Thurm, A., & Pickles, A. (2006). Autism from 2 to 9 years of age. Archives of general psychiatry, 63(6), 694–701. https://doi.org/10.1001/archpsyc.63.6.694
National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention. (2016). Autism Spectrum Disorder (ASD): Data & Statistics. Centers for Disease Control. https://www.cdc.gov/autism/data-research/?CDC_AAref_Val=https://www.cdc.gov/ncbddd/autism/data.html
Nei, M., Ngo, L., Sirven, J. I., & Sperling, M. R. (2014). Ketogenic diet in adolescents and adults with epilepsy. Seizure, 23(6), 439–442. https://doi.org/10.1016/j.seizure.2014.02.015
Norton, E. S., & Wolf, M. (2012). Rapid automatized naming (RAN) and reading fluency: implications for understanding and treatment of reading disabilities. Annual review of psychology, 63, 427–452. https://doi.org/10.1146/annurev-psych-120710-100431
Ozernov-Palchik, O., & Gaab, N. (2016). Tackling the 'dyslexia paradox': reading brain and behavior for early markers of developmental dyslexia. Wiley interdisciplinary reviews. Cognitive science, 7(2), 156–176. https://doi.org/10.1002/wcs.1383
Ozonoff, S., Young, G. S., Carter, A., Messinger, D., Yirmiya, N., Zwaigenbaum, L., Bryson, S., Carver, L. J., Constantino, J. N., Dobkins, K., Hutman, T., Iverson, J. M., Landa, R., Rogers, S. J., Sigman, M., & Stone, W. L. (2011). Recurrence risk for autism spectrum disorders: a Baby Siblings Research Consortium study. Pediatrics, 128(3), e488–e495. https://doi.org/10.1542/peds.2010-2825
Papavassiliou, P., Charalsawadi, C., Rafferty, K., & Jackson-Cook, C. (2015). Mosaicism for trisomy 21: a review. American journal of medical genetics. Part A, 167A(1), 26–39. https://doi.org/10.1002/ajmg.a.36861
Paulesu, E., Danelli, L., & Berlingeri, M. (2014). Reading the dyslexic brain: multiple dysfunctional routes revealed by a new meta-analysis of PET and fMRI activation studies. Frontiers in human neuroscience, 8, 830. https://doi.org/10.3389/fnhum.2014.00830
Presson, A. P., Partyka, G., Jensen, K. M., Devine, O. J., Rasmussen, S. A., McCabe, L. L., & McCabe, E. R. (2013). Current estimate of Down Syndrome population prevalence in the United States. The Journal of pediatrics, 163(4), 1163–1168. https://doi.org/10.1016/j.jpeds.2013.06.013
Schendel, D., & Bhasin, T. K. (2008). Birth weight and gestational age characteristics of children with autism, including a comparison with other developmental disabilities. Pediatrics, 121(6), 1155–1164. https://doi.org/10.1542/peds.2007-1049
Thapar, A., Cooper, M., Eyre, O., & Langley, K. (2013). What have we learnt about the causes of ADHD?. Journal of child psychology and psychiatry, and allied disciplines, 54(1), 3–16. https://doi.org/10.1111/j.1469-7610.2012.02611.x
Tolaymat, A., Nayak, A., Geyer, J. D., Geyer, S. K., & Carney, P. R. (2015). Diagnosis and management of childhood epilepsy. Current problems in pediatric and adolescent health care, 45(1), 3–17. https://doi.org/10.1016/j.cppeds.2014.12.002
Tomasi, D., & Volkow, N. D. (2014). Functional connectivity of substantia nigra and ventral tegmental area: maturation during adolescence and effects of ADHD. Cerebral cortex (New York, N.Y. : 1991), 24(4), 935–944. https://doi.org/10.1093/cercor/bhs382
Visser, S. N., Danielson, M. L., Bitsko, R. H., Holbrook, J. R., Kogan, M. D., Ghandour, R. M., Perou, R., & Blumberg, S. J. (2014). Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003-2011. Journal of the American Academy of Child and Adolescent Psychiatry, 53(1), 34–46.e2. https://doi.org/10.1016/j.jaac.2013.09.001
Willsey, A. J., & State, M. W. (2015). Autism spectrum disorders: from genes to neurobiology. Current opinion in neurobiology, 30, 92–99. https://doi.org/10.1016/j.conb.2014.10.015
Wiseman, F. K., Al-Janabi, T., Hardy, J., Karmiloff-Smith, A., Nizetic, D., Tybulewicz, V. L., Fisher, E. M., & Strydom, A. (2015). A genetic cause of Alzheimer disease: mechanistic insights from Down syndrome. Nature reviews. Neuroscience, 16(9), 564–574. https://doi.org/10.1038/nrn3983
Witton, J., Padmashri, R., Zinyuk, L. E., Popov, V. I., Kraev, I., Line, S. J., Jensen, T. P., Tedoldi, A., Cummings, D. M., Tybulewicz, V. L. J., Fisher, E. M. C., Bannerman, D. M., Randall, A. D., Brown, J. T., Edwards, F. A., Rusakov, D. A., Stewart, M. G., & Jones, M. W. (2015). Hippocampal circuit dysfunction in the Tc1 mouse model of Down syndrome. Nature neuroscience, 18(9), 1291–1298. https://doi.org/10.1038/nn.4072
Young, L. J., & Barrett, C. E. (2015). Neuroscience. Can oxytocin treat autism? Science (New York, N.Y.), 347(6224), 825–826. https://doi.org/10.1126/science.aaa8120
Zuberi, S. M., & Symonds, J. D. (2015). Update on diagnosis and management of childhood epilepsies. Jornal de pediatria, 91(6 Suppl 1), S67–S77. https://doi.org/10.1016/j.jped.2015.07.003