Tackling Alzheimer’s from Bench to Bedside with Takeshi Iwatsubo
- Published5 Aug 2025
- Author Bella Isaacs-Thomas
- Source BrainFacts/SfN

Alzheimer’s disease researchers are in a race against time to improve outcomes for patients. Around 60 million people across the globe currently have dementia, of which Alzheimer’s is the most common cause. In the coming decades, cases of the disease are projected to balloon, especially in countries with aging populations. But major breakthroughs in recent years have led to novel therapies developed to target the disease, new ways to diagnose it, and clearer understandings of how it plays out in the brain.
“Particularly in the last two decades, the acceleration has been tremendous,” said Eric McDade, a neurologist and researcher at Washington University in St. Louis.
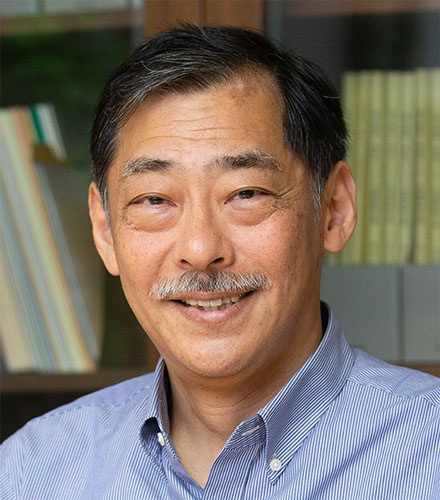
Few experts in this field have directly or indirectly touched the lives of so many patients as Takeshi Iwatsubo, a professor of neuropathology at the University of Tokyo Graduate School of Medicine and director of Japan’s National Institute of Neuroscience and the National Center for Neurology and Psychiatry. A neurologist by training, Iwatsubo’s career has straddled the worlds of basic neuroscience in the lab and real-world clinical trials.
Iwatsubo played a pivotal role in trials evaluating first-of-their-kind therapeutics that slow Alzheimer's progression by targeting toxic protein buildup associated with the disease. These drugs mark the dawn of a new era of Alzheimer's care, but the work is far from complete. People across the globe face limited access to these therapeutics, and researchers are continuing to search for treatments which could completely stop or reverse patients’ symptoms.
Still, after decades of experience in multiple facets of the field, Iwatsubo emphasizes how groundbreaking this development is for patients and providers. Now, “they have the hope not for the perfect cure, but the slowdown of the progression,” Iwatsubo said. “So that is impressive — remarkable.”
Game-Changing Therapeutics
Alzheimer’s disease is characterized by the toxic buildup of two proteins in the brain — amyloid beta and tau. Researchers suspect amyloid beta accumulation, which is toxic to neurons, marks the earliest stages of the disease. As it progresses, Iwatsubo explained, growing tau deposits between cells eventually serve as a secondary catalyst of the neuronal death which fuels cognitive decline.
“Amyloid beta may be the driver as well as the upstream trigger of the neurodegenerative process,” Iwatsubo said. “And tau may be more like a driver, so it accelerates the neurodegeneration.”
The two therapeutics available to patients today — donanemab and lecanemab — work by removing built-up amyloid deposits in the brain. The drugs don’t cure Alzheimer’s, but they can reduce the speed of symptom progression by 30%. Ongoing trials are evaluating drugs which target tau accumulation, too. One day, patients could have access to a combination of therapies targeting amyloid beta and tau to further stymie Alzheimer’s progression.
Now, Iwatsubo is setting up a patient registry in Japan to evaluate their real-world efficacy and safety by collecting data from people taking anti-amyloid drugs. Sister programs in the United States and Europe will also collect this information. This collaboration allows participating nations to benefit from a massive dataset, paving the way for robust analysis of their combined findings.
Identifying Biomarkers
By and large, Alzheimer’s researchers envision a future where the root causes of the disease can be pharmacologically nipped in the bud. Amyloid beta builds up in the brain for decades before patients begin to demonstrate noticeable symptoms, like memory loss. The hope is patients could one day take drugs to reduce amyloid levels, or even tau levels, before they experience mass, irreversible neuron degeneration.
“I think all of us in the field think that eventually with Alzheimer's disease, it'll be like a lot of other chronic diseases that you have multiple therapies that you need to treat the different aspects of it,” McDade said.
But before patients can gain access to therapeutics, they must first receive a diagnosis. Early Alzheimer’s detection hinges on the development of biomarkers, or molecular indicators of the disease.
Chihiro Sato, an assistant professor of neurology also based at Washington University in St. Louis, studies tau pathology in Alzheimer’s and other diseases. Her goal is to evaluate how the protein can be used as an indicator of where patients are in their disease progression and in clinical trials to measure the efficacy of new therapeutics.
Today, physicians typically diagnose Alzheimer’s disease by using a PET scan or a spinal tap to confirm amyloid beta buildup in patients’ brains. But these pricey diagnostic tests can be difficult for many patients to access. In May of 2025, the FDA approved the first blood test designed to flag this protein, a comparatively cheaper and faster approach. Scientists hope future tests like this one could help ease the diagnosis process for patients while also helping providers catch the disease as early as possible.
Early detection is also key to getting existing therapeutics in patients’ hands while they’re still effective at slowing the disease. “Amyloid-beta targeted therapies are more effective for people at the earlier stage,” Sato said. “And if you go way beyond, then this amyloid therapy doesn't work because amyloid has already built up and killed neurons, and you can't beat a dead horse.” In an ideal world, she added, people would have access to simple Alzheimer’s screenings to catch biomarkers before they’ve done significant damage to the brain.
Where Does Alzheimer’s Research Go from Here?
Sato worked in Iwatsubo’s lab at the University of Tokyo while pursuing her master’s degree and PhD, where she was drawn to the “bench to bedside” nature of his work. As she pursues basic neuroscience research in her own lab, she remains attuned to how discoveries like hers will affect “people and families” who are suffering due to Alzheimer’s.
“Dr. Iwatsubo is legendary. I don’t think anybody [else] can be like him [in the future of Alzheimer’s research,]” Sato said. “He has been in this very dramatic period where many key discoveries have been made at the basic level and all the way to the clinic.”
Many Alzheimer’s breakthroughs were made possible by long-term, intensive research involving people with exceedingly rare, hereditary forms of the disease. A handful of families across the globe pass down genetic mutations that lead to an overproduction of particularly sticky types of amyloid beta, plus the downstream phenomenon of tau-fueled neurodegeneration, Iwatsubo explained.
These cases make up a miniscule fraction of Alzheimer’s patients. For 99% of patients, he said, the root cause of their condition isn’t clear. Risk factors related to people’s environments, the aging process itself, and more common genetic predispositions all play a role in disease onset. But Iwatsubo noted the specific “molecular mechanisms” driving their pathology remains uncertain.
Both Iwatsubo and McDade have been involved with the Dominantly Inherited Alzheimer’s Network (DIAN), an international research effort which studies people with highly rare forms of the disease. Networks like these aren’t possible without multi-national collaboration and funding from public and private sources. In the U.S., the Trump administration has wiped out multiple funding sources originally allocated to support a vast range of biomedical research efforts. McDade expressed alarm over what those cuts could mean for patients involved in ongoing clinical trials, and for the broader message the abdication of this work could send to the rest of the world.
“I have, at this point, increasing concerns about the potential threat that this has on Alzheimer's disease research at a time when we've honestly never been more optimistic for those who are in the field and doing this research,” McDade said.
CONTENT PROVIDED BY
BrainFacts/SfN
References
Chen, C., Katayama, S., Lee, J. H., Lee, J. Y., Nakagawa, M., Torii, K., Ogawa, T., Dash, A., Irizarry, M., Dhadda, S., Kanekiyo, M., Hersch, S., & Iwatsubo, T. (2025). Clarity AD: Asian regional analysis of a phase III trial of lecanemab in early Alzheimer's disease. The Journal of Prevention of Alzheimer's Disease, 12(5), 100160. https://doi.org/10.1016/j.tjpad.2025.100160
Horie, K., Salvadó, G., Koppisetti, R. K., Janelidze, S., Barthélemy, N. R., He, Y., Sato, C., Gordon, B. A., Jiang, H., Benzinger, T. L. S., Stomrud, E., Holtzman, D. M., Mattsson-Carlgren, N., Morris, J. C., Palmqvist, S., Ossenkoppele, R., Schindler, S. E., Hansson, O., & Bateman, R. J. (2025). Plasma MTBR-tau243 biomarker identifies tau tangle pathology in Alzheimer's disease. Nature Medicine, 31(6), 2044–2053. https://doi.org/10.1038/s41591-025-03617-7
Iwatsubo, T. (2024). Development of disease-modifying therapies against Alzheimer's disease. Psychiatry and Clinical Neurosciences, 78(9), 491–494. https://doi.org/10.1111/pcn.13681
Iwatsubo, T. (2023). Editorial: Clinical Implementation of Lecanemab: Challenges, Questions and Solutions. The Journal of Prevention of Alzheimer's Disease, 10(3), 353–355. https://doi.org/10.14283/jpad.2023.41
McDade, E., Hake, A. M., Bain, L. J., & Carrillo, M. (2019). Targeting Alzheimer's Disease in the Preclinical Stage. Alzheimer's and Dementia, 15(4), 602-603. https://doi.org/10.1016/j.jalz.2019.03.008
Nakashima, S., Sato, K., Niimi, Y., Ihara, R., Suzuki, K., Iwata, A., Toda, T., Iwatsubo, T., & Alzheimer's Disease Neuroimaging Initiative (2025). Therapeutic time window of disease-modifying therapy for early Alzheimer's disease. Alzheimer's & Dementia (New York, N. Y.), 11(2), e70102. https://doi.org/10.1002/trc2.70102
Sato, K., Niimi, Y., Ihara, R., Iwata, A., Suzuki, K., & Iwatsubo, T. (2025). Blood-based biomarker prescreening with different testing combinations and cutoffs: A simulation study examining efficacy and cost-effectiveness in Alzheimer's disease prevention studies. Alzheimer's & Dementia (New York, N. Y.), 11(1), e70065. https://doi.org/10.1002/trc2.70065
Wang, G., Berry, S., Xiong, C., Hassenstab, J., Quintana, M., McDade, E. M., Delmar, P., Vestrucci, M., Sethuraman, G., Bateman, R. J., & Dominantly Inherited Alzheimer Network Trials Unit (2018). A novel cognitive disease progression model for clinical trials in autosomal-dominant Alzheimer's disease. Statistics in Medicine, 37(21), 3047–3055. https://doi.org/10.1002/sim.7811
What to Read Next
Also In Supporting Research
Trending
Popular articles on BrainFacts.org


.jpg)