A Perceptive Lens: Marlene Behrmann
- Published11 Mar 2020
- Author Kayt Sukel
- Source BrainFacts/SfN
When a premature detonation of explosives drove a tamping iron clear through Phineas Gage’s head, his drastically altered behavior and personality allowed doctors to understand the role of the brain’s frontal lobe in executive control. Paul Broca’s “Tan,” possessed damage on the left side of his temporal lobe, revealing how the brain processes language. And H.M., probably the most famous neuroscience study participant, allowed Donald Hebb and Brenda Milner to establish the foundational principles of human memory. But you may be less aware of patient L.M., who viewed the world in static “snapshots,” unable to perceive motion.
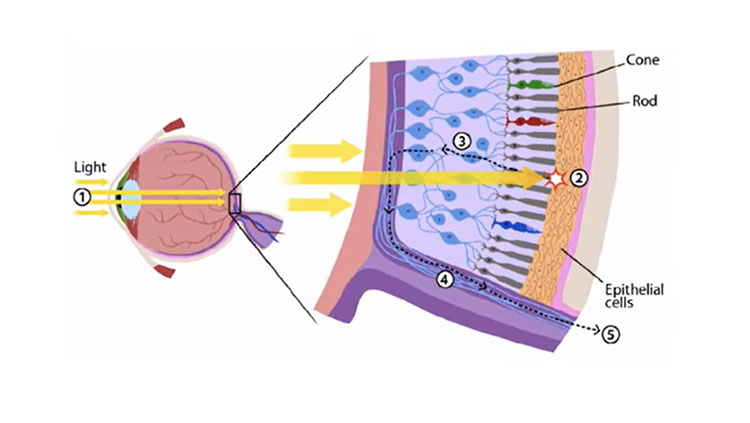
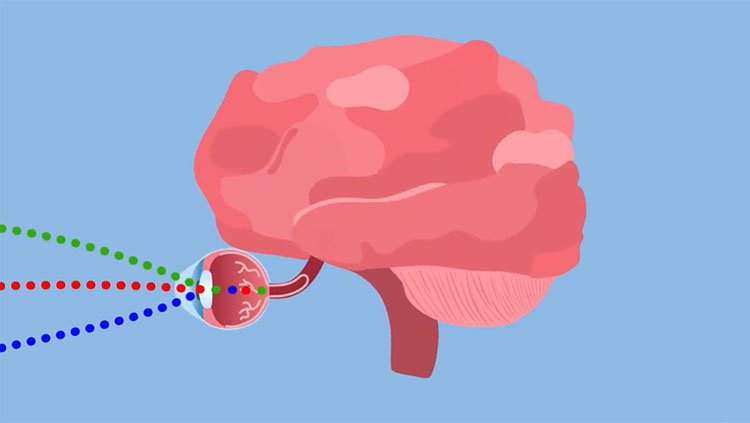
Our understanding of visual perception has been built on the brains of hundreds of patients who had focal lesions or damage sustained in their visual cortex, located in the back of the brain in the occipital lobes.
Marlene Behrmann, a cognitive scientist at Carnegie Mellon University, has spent her career studying the cognitive basis of visual perception. Her most recent work shows that children who undergo brain surgery for severe epilepsy, involving the removal of a portion of one side of the visual cortex, keep almost full visual perception capabilities.
What, historically, have we learned about the human visual system from patients?
We’ve learned that visual function requires not only the sensory information that comes in from the eye but various parts of the brain, including the primary visual cortex and higher levels of visual cortex, to help us recognize patterns, objects, faces, and words. There are a variety of dramatic neuropsychological disorders that tell us the brain processes information about these things quite differently:
• Prosopagnosia: these patients often struggle with recognizing the face of any family members or even a photograph of themselves.
• Alexia: these patients essentially lose the ability to recognize any written material.
• Hemispatial neglect takes away the ability of patients to pay attention to one side of the visual field.
There is even a condition called blindsight: patients have no damage to their eyes but are blind as a result of focal damage to the visual cortex, yet they can respond to visual stimuli. The brain appears to be taking in at least some information about what these patients are seeing. For example, patients can make discriminations about the visual stimuli even as they tell you they see nothing. Studying these abnormalities, caused by damage to different parts of visual cortex, helps us to understand how the brain is organized. As we lay out a theoretical foundation for how the visual system works, we need to be able to account for individuals with normal visual perception as well as be able to explain the nature of these selective deficits.
Your recent work has looked at children with epilepsy who have undergone a hemispherectomy, or a resection of an entire hemisphere in the visual cortex. What did you find?
Remarkably, even after the removal of the occipital and temporal cortex in one hemisphere, these children show almost no perceptual deficits in tasks involving facial recognition, reading, pattern recognition, or in their ability to recognize and classify objects. Many did exhibit visual field deficits or lose vision in one visual field (e.g. all information that falls, for example, to the left of the nose when one is looking forward after a right hemisphere surgical resection). But, for the most part, their abilities for perceptual tasks fell well within the normal range. When we used neuroimaging to look at brain activity, we saw that even tasks that, in healthy adults, are more dominant in one hemisphere, like word recognition in the left hemisphere, remapped over to the other side of the brain. The remaining hemisphere was able to compensate for that missing tissue.
Past research suggests that both the left and right hemisphere play a dominant — but not exclusive — role in certain processes like word recognition and face recognition, respectively. But our work suggests that a single hemisphere is rather good at taking on the role of both hemispheres without much cost to perceptual function.
However, it raises a very important question: what allows for this kind of reorganization across the hemispheres in children that we don’t see in adults? What’s behind this kind of neuroplasticity? Certainly, it is maybe due, in part, to the fact these children’s brains are still developing. It’s also likely the reorganization happened much, much earlier, in response to their epilepsy. We don’t know yet. There’s a lot of work to be done in thinking about how to use these results to make the kind of inferences that can tell us something about how the normal visual system works and how it rewires itself in response to injury.
CONTENT PROVIDED BY
BrainFacts/SfN
Also In Vision
Trending
Popular articles on BrainFacts.org