The Neural Regulation of Thirst
- Published16 Mar 2008
- Reviewed16 Mar 2008
- Author Susan Perry
- Source BrainFacts/SfN
Everybody gets thirsty. The urge to drink fluids is a natural instinct regulated by a negative feedback loop between the brain and other organs in the body. In the elderly and others, however, that loop sometimes weakens, putting their health dangerously at risk. By unraveling the complexity of the thirst mechanism, scientists are developing better treatments for people who lose their sense of thirst and are gaining greater knowledge about many other basic human behaviors.
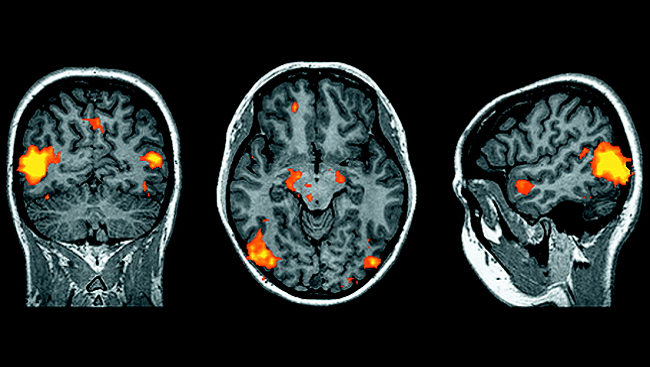
The positron emission tomography (PET) image at top, taken after subjects received an infusion of a concentrated saline solution into the blood to stimulate thirst, shows regions of activity in the left side of the brain in thirsty subjects. This activity changed dramatically after their thirst was quenched. In particular, the yellow and orange areas above indicate activity along the cingulate cortex that was extinguished later.
Thirst. As far as survival instincts go, it doesn’t get more basic. Water is the most abundant molecule in the human body, making up about 70 percent of our body weight. It performs a host of important internal functions, from maintaining body temperature; to transporting vitamins, minerals, hormones, and other substances; to lubricating joints, eyes, and intestines.
We can survive for only a matter of days without water. Thirst serves as an automatic reminder of that fact—and, thus, plays a crucial role in keeping us alive.
Yet people sometimes lose their sense of thirst. The elderly in particular are prone to not feeling thirsty, even as they become dehydrated. Certain brain injuries also can prevent people from recognizing when they need to drink.
Recently, reports of people, particularly marathon runners, who drink too much water in an overzealous attempt to avoid dehydration have hit the news. The excess water overwhelms the kidneys, which can’t flush out the fluid fast enough. The water then rushes into cells throughout the body, swelling them like balloons. In the brain, such swelling can be disastrous, causing seizures, coma, respiratory arrest, and death.
Recent research is helping scientists gain greater knowledge about thirst and the brain’s role in regulating it. These studies are leading to:
- A better understanding of how aging mutes the sense of thirst.
- Greater insight into diabetes insipidus (“water” diabetes) and other diseases for which excessive thirst is a symptom.
- Safer recommendations for how much water marathon runners and others engaged in endurance exercise should consume.
Scientists have been studying the neurological mechanisms of thirst for decades. Early on, they discovered that the body’s primary “thirst center” in the brain is the hypothalamus, a deep structure that also regulates body temperature, sleep, and appetite. Special sensors in the hypothalamus are constantly monitoring the blood’s concentration of sodium and other substances. The hypothalamus also receives inputs from sensors in the blood vessels that monitor blood volume and pressure. When blood volume or pressure falls too low—from bleeding, for example, or from the excessive loss of fluid in sweat or diarrhea, or when blood sodium concentration rises too high from eating salty snacks, or as the result of certain diseases, the hypothalamus sends out a strong message: Drink something. Now.
For reasons that aren’t clear, age tends to dampen this message from the brain. In rare cases, when an aneurysm or other brain injury has destroyed the sensors in the hypothalamus that regulate blood sodium concentration, people can lose their sense of thirst completely. They must be prescribed a fixed amount of fluids daily to keep their body safely hydrated.
Thirst isn’t the brain’s only response to dehydration. When the body gets low on water, the hypothalamus increases the synthesis of an antidiuretic hormone called vasopressin, which is secreted by the pituitary gland and travels to the kidneys. There, it causes water to be reabsorbed from the urine, thus reducing urine flow and conserving water in the body until more fluids are consumed.
If the pituitary gland becomes damaged, however, or if the kidneys are unable to respond to vasopressin, the body is unable to conserve fluids. The result can be diabetes insipidus, a condition marked by excessive urination and extreme, uncontrollable thirst. (Diabetes insipidus should not to be confused with diabetes mellitus, which also causes excessive thirst and urination, but which results from an insulin deficiency or resistance that leads to high blood glucose.)
Until scientists understood the structure of vasopressin and its role in diabetes insipidus, people with the condition had to drink up to 20 quarts of water daily to stay healthy. Today, however, diabetes insipidus can be successfully treated with the synthetic drug demopressin, which mimics the action of vasopressin.
Recently, scientists have discovered that vasopressin secretion increases (and, thus, less body fluid is lost) during periods of physical stress. For that reason, many medical experts are now recommending that healthy runners drink only when thirsty during marathons to avoid retaining excess water with potentially dire consequences.
Although much has been learned about the neural regulation of thirst, research continues. Scientists are exploring, for example, why such factors as swallowing and the emptying of fluids from the stomach appear to inhibit thirst even before the body becomes fully hydrated. Studies into the thirst mechanism also are helping unravel some of the mechanisms by which the brain motivates sleep, appetite, and other basic human instincts.
CONTENT PROVIDED BY
BrainFacts/SfN
Also In Archives
Trending
Popular articles on BrainFacts.org