It Takes a Village: Large-Scale Studies Prove Vital to Alzheimers Disease Research
- Published1 Dec 2010
- Reviewed1 Dec 2010
- Source The Dana Foundation
Richard Hodes, M.D. National Institute on aging and the variations that make researching Alzheimer's so difficult.
During the next 25 years, the number of Americans living to age 65 is expected to double to about 72 million. Many people thrive as they age, but others experience cognitive decline wrought by Alzheimer’s disease and other dementias. Today, as many as 5.1 million Americans may have Alzheimer’s disease, the most common form of dementia. Unless we can cure or prevent it, Alzheimer’s prevalence may triple by 2050.
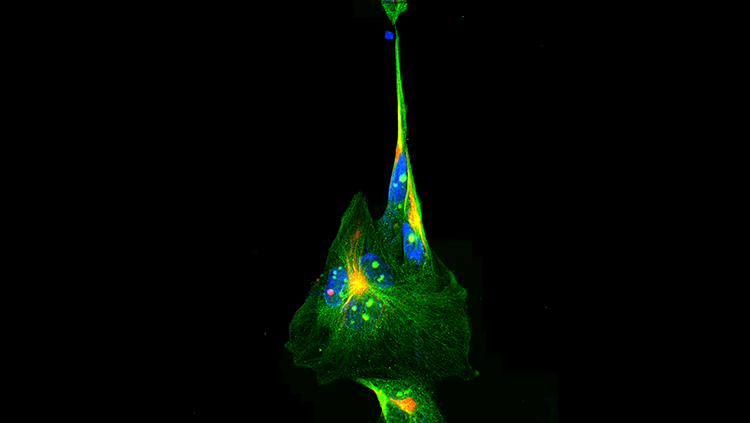
These dire projections lend urgency to research into this devastating disease. In the past decade, researchers and clinicians working across diverse disciplines have made important discoveries about the molecular changes that take place in the brains of people with Alzheimer’s disease, identified genetic risk factors, and pointed to lifestyle and environmental factors—such as diet and exercise—that may contribute to the onset and progression of the disorder.
Along with these advances, however, came a humbling appreciation of the complexity of Alzheimer’s. More than a century since Alois Alzheimer first described abnormal deposits of beta-amyloid and tau proteins in the brain of a woman with dementia, researchers are still asking if these hallmark plaques and tangles are the causes or the results of the disease process. While it is difficult to predict when we will have the answers, we may gain great insight from large-scale, collaborative studies.
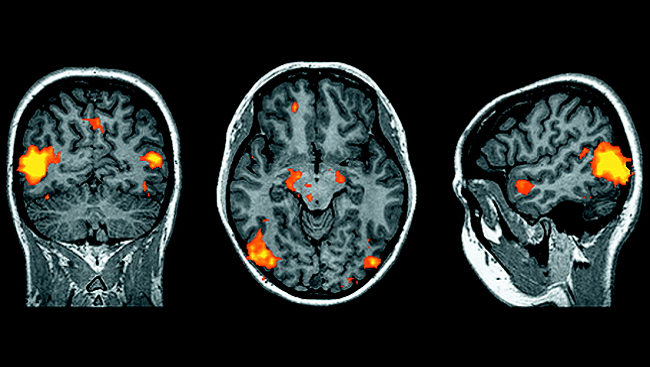
Researchers in government, academia and private industry are joining forces to discover the genetic and environmental risk factors involved in Alzheimer’s. One such success story is the Alzheimer’s Disease Neuroimaging Initiative (ADNI), a partnership launched in 2004 and primarily supported by the National Institute on Aging (NIA), joined by other NIH institutes and private partners. ADNI scientists are developing imaging and biomarker profiles of the changes that signal the onset of Alzheimer’s, sometimes long before symptoms appear.
These new biomarker tools—from brain scans to blood and cerebrospinal fluid tests—will enable us to detect and follow the progression of Alzheimer’s during clinical trials. And the scientists’ efforts are beginning to show results. In spring 2009, ADNI reported that certain cerebrospinal fluid biomarkers may help us both predict who is at risk of developing the disease and learn how the disease responds to various therapies. These data, involving hundreds of volunteers, are available to qualified researchers worldwide, thus further driving the collaborative nature of the research and strengthening our chances of finding answers quickly. Ultimately, we hope that these technologies will prove useful in everyday clinical practice so that we can implement therapies or preventative measures as soon as possible.
We anticipate that a similar collaborative approach will tell us more about Alzheimer’s risk factor genes. Researchers have shown thatthree genes cause the rare, early-onset form of Alzheimer’s that occurs in some families. However, only one of the other 30,000 genes in our DNA is linked to increased risk for the more widespread, late-onset form that commonly occurs after age 65. Scientists are eager to identify additional risk factor genes.
Genome-wide association studies, which use methods that can rapidly test up to a million sites in one person’s genes, will help scientists find those elusive genetic variations. Since 2007, several international research groups conducting association studies have identified variants of the SORL1, CLU, PICALM and CR1 genes that may play a role in the risk of late-onset Alzheimer’s.
To build the large bank of DNA samples needed for future association studies, the NIA supports the Alzheimer’s Disease Genetics Consortium, which collects and analyzes biological samples from tens of thousands of people with and without the disease. The consortium freely shares its data and analyses with others in the research community to help spur advances in our understanding of the genetic mechanisms at work and to help scientists identify new pathways to prevention or treatment.
The past decade is also marked by advances in translational research—applying knowledge gained in the laboratory as quickly as possible to new tests or therapies in a clinical setting. The NIA currently supports 60 grants aimed at identifying and developing effective therapies for the treatment of Alzheimer’s. The work is varied, from finding new compounds that will modify beta-amyloid production or clear it from the brain to reformulating existing drugs and naturally occurring compounds used to treat other diseases. These studies allow the NIA to capture new and creative therapeutic approaches and to “seed” promising drug discovery and preclinical development programs.
The success of these and many other efforts relies on another vital partner in Alzheimer’s research: the many volunteer research participants, including patients in clinical trials. Both our recent progress and our growing confidence for future advances rely heavily on this generosity of spirit. Collaboration is key to translating discoveries into safe and effective therapies that will benefit us all. For information about volunteering, visit: https://www.researchmatch.org.
CONTENT PROVIDED BY
The Dana Foundation is a private philanthropic organization that supports brain research through grants and educates the public about the successes and potential of brain research.
Also In Archives
Trending
Popular articles on BrainFacts.org