Understanding Mental Disorders as Circuit Disorders
- Published1 Dec 2010
- Reviewed25 Mar 2014
- Source The Dana Foundation
Tom Insel, M.D., National Institute of Mental Health on an alternate way to look at mental disorders.
When the Decade of the Brain began in 1990, scientists had developed both drug and behavioral treatments for most mental disorders, but their understanding of these disorders was primitive. Two decades later, neuroscientists are finally uncovering the brain processes involved in mental disorders. There is great promise for development of more effective treatments in the upcoming decade.
In 1990, most theories of the causes of mental disorders were based on investigations of treatments, rather than on scientific insight about how diseases arise. By 2000, we had developed more treatments—including best-selling second-generation antipsychotics and antidepressants—but we were no further along in our understanding of the causes. During the so-called Decade of the Brain, there was neither a marked increase in the rate of recovery from mental illness, nor a detectable decrease in suicide or homelessness—each of which is associated with a failure to recover from mental illness. To reduce the occurrence and death toll of mental disorders, we will need a more thorough understanding of why these mysterious illnesses occur.
People frequently cite the 1990s as the era for redefining mental disorders as brain disorders. While this conceptual shift was important, we now realize the greater importance of developing new tools: imaging techniques for quantitative studies of brain structure, function and chemistry, as well as other comprehensive tools for mapping DNA and RNA. What do we mean by comprehensive? Rather than focusing on four or five neurotransmitters, researchers at the turn of the 21st century were able to investigate thousands of genes to yield an unbiased survey of the biology of mental disorders. These advances ushered in a decade of discovery that brings us to 2010.
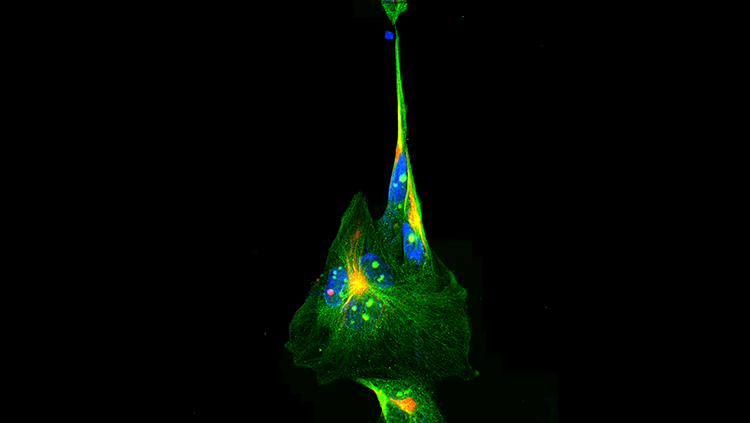
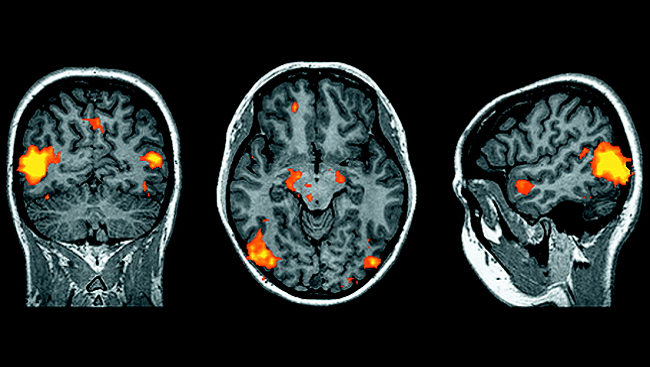
If scientists introduced mental disorders as brain disorders in the Decade of the Brain, researchers in the past ten years have demonstrated the importance of specific brain circuits. Unlike neurological disorders, which often involve areas of tissue damage or cell loss, mental disorders have begun to appear more like circuit disorders, with abnormal conduction between brain areas rather than loss of cells.
Neuroimaging technology has revealed that specific brain pathways, mostly located in the prefrontal cortex, are involved in major mental disorders. Deep brain stimulation, a procedure in which neurologists manipulate certain pathways via electric current, has shown promise as a treatment for depression and obsessive-compulsive disorder, on the heels of its successful use as a treatment for neurological motor disorders such as Parkinson’s. In the past couple of years, via a new technology called optogenetics, neuroscientists have used light to manipulate circuits in experimental animals with millisecond precision and cellular resolution. Thus, for the first time, researchers can conduct specific tests of theories about brain circuits and behavior.
What causes a circuit disorder? Although this will be a major question for the next decade, we already have some intriguing ideas. Mental disorders such as schizophrenia and mood and anxiety disorders are mostly diseases of early life; their onset tends to occur during adolescence or early adulthood, when the brain is still developing. For example, a person with schizophrenia usually experiences a psychotic break in early adulthood, which is a time when the number of cortical synapses is being pruned. The disorder might result from the excessive loss of synapses in a critical cortical pathway when the normal process overshoots.
Since 2005, scientists studying our genes, the proteins they produce and their functions have started to identify some of the key factors that increase the risk of mental disorders, from autism toschizophrenia. The candidates include a long list of previously unknown proteins that have one thing in common: They are important for healthy brain development. Indeed, if the Decade of the Brain redefined mental disorders as brain disorders, recent research suggests that mental disorders are really developmental brain disorders, caused by disruptions in the circuitry map of the developing brain.
During this next decade, expect to see the full roster of candidates as scientists begin to describe the key variations in sequences of genes that produce altered proteins and dysfunctional circuitry. Neuroscientists already have powerful tools to move from the study of molecules to circuits and, ultimately, to behavior. How will we translate this emerging knowledge into better treatments? The answer for psychiatry will likely be the same as the answer in the rest of medicine: Basic discoveries regarding genes and proteins will point the way to molecular and cellular mechanisms, which in turn will yield new targets for treatment and prevention.
In some ways, psychiatry has been the victim of its early success, as medications found by accident in the 1960s delayed the search for fundamental mechanisms of disease that could yield new targets and new treatments. After two decades of progress, clinical neuroscientists are finally beginning to understand what underlies a few mental disorders. In the upcoming decade, which we can perhaps call the Decade of Translation, we can look forward to seeing this new understanding translate to improved treatments that will finally reduce the occurrence and death rates of these disabling illnesses.
CONTENT PROVIDED BY
The Dana Foundation is a private philanthropic organization that supports brain research through grants and educates the public about the successes and potential of brain research.
Also In Archives
Trending
Popular articles on BrainFacts.org