New Diagnostic Criteria for Alzheimer’s Disease: What do they really mean?
- Published1 Aug 2011
- Reviewed1 Aug 2011
- Source The Dana Foundation
In April 2011, new diagnostic criteria for Alzheimer’s disease (AD) were published, revising criteria that had been in place for 27 years. The new criteria are important because they shift the focus in clinical research to detecting the disease as early as possible, optimally prior to the onset of dementia. David M. Holtzman, M.D., Washington University School of Medicine, St. Louis, explains what this means for future patients.
Major scientific advances in genetics, biochemistry, cell biology, and neuroscience over the past 30 years have led to the hope that, if the brain changes that cause AD can be detected before a person becomes demented, it is likely that exciting new treatments being developed can and will be effective. This hope is reflected in the new AD diagnostic criteria, where the two most important features are the formal identification of different stages of the disease and the addition of the concept and use of biomarkers that can reveal the underlying cause of a disease state.
What is dementia?
Dementia refers to the loss of memory and thinking abilities sufficient to impair social and occupational function. It is extremely common with aging, affecting about 4 percent of the population by age 70 and roughly 50 percent of the population age 85 and greater. AD is the most common cause of dementia, contributing to about 75 percent of cases. Today, dementia affects about 30 million people worldwide. This number is expected to quadruple in 40 years unless a treatment that prevents of delays the disease is developed. Currently, no treatment delays the onset or slows the progression of AD.
During healthy aging, it is normal to have some trouble with word-finding, particularly for names, as well as note some mild slowing of thinking processes. However, it is not normal to become repetitious, to forget recent conversations, or to become disoriented in familiar places. These are some of the signs that can characterize AD. If such problems are relatively mild and not yet interfering strongly with normal activities, they are sometimes referred to as very mild dementia or mild cognitive impairment (MCI)
The pathological and clinical time course of AD
In the past quarter-century, many key scientific, clinical, and pathological discoveries have told us much about AD in its different stages, including the very mild dementia/MCI stage. Several key changes in the brain characterize AD and play an important role in nerve cell degeneration. Abundant evidence suggests that the accumulation in the brain of proteins called amyloid-β (Aβ for short) and tau ultimately lead to a series of events—including inflammation, neuron loss, and loss of parts of nerve cells that communicate called synapses—culminating in the cognitive syndrome we know as AD. Best estimates are that the gradual accumulation of Aβ in the brain begins roughly 10–15 years before the onset of any signs or symptoms of cognitive decline and that, by the time someone is demented, the amount of this protein that has built up in the brain is near its maximal extent. The tau protein begins to accumulate in the regions of the brain responsible for many cognitive functions, called the neocortex, about 5 years prior to cognitive decline.
The accumulation of these two proteins in the brain damages nerve cells and their connections. However, the human brain seems to have a fair amount of what is termed “cognitive reserve” to withstand damage caused by these proteins for a long time before nerve cells and synapses degenerate to the point that memory loss and decline in other cognitive skills are noted by friends and family.
In other words, by the time even very mild dementia/MCI is apparent, if it is due to AD, substantial nerve cell and synaptic loss has already occurred, but patients are not yet impaired enough to meet the old formal criteria for an AD diagnosis. The old criteria were that a patient’s decline in recent memory and at least one other area of cognitive abilities was sufficient to significantly impair occupational or social functioning. Scientists and clinicians realized that AD’s assault on the brain must be fought when an individual is still cognitively normal, and they needed to develop new criteria to diagnose AD before even the most subtle cognitive impairment, for both clinical and research purposes.
How can one be sure that AD is occurring in the presence or absence of symptoms?
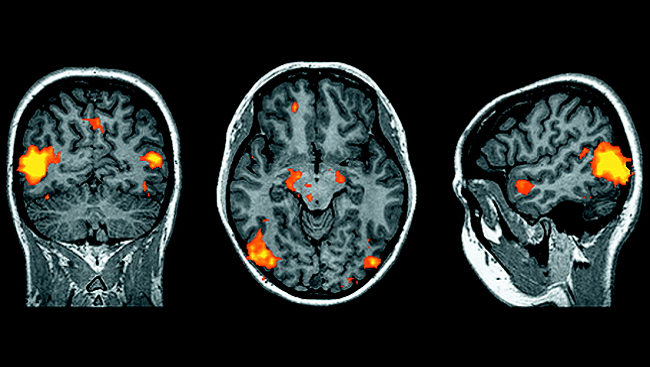
A major change in both diagnosing and predicting outcome in AD has come from the use of biomarkers. Biomarkers are signs or substances that can be measured in the body (e.g. using imaging, blood, spinal fluid) and reflect specific processes related to disease. Some AD biomarkers include proteins that can be measured in the cerebrospinal fluid and the presence or absence of Aβ and tau accumulations in the brain, which certain imaging methods can now detect. Other biomarkers can be obtained using magnetic resonance imaging (MRI) and positron emission tomography (PET); for example, scans can determine if brain tissue is of normal size or if damage and loss of nerve cells and their connections have occurred. With such tools in hand, we can now determine if the pathology of AD is present or absent in an individual who is either cognitively impaired or is cognitively normal.
While more research needs to be done on these biomarkers and how to precisely interpret their meaning, their identification has led to a conceptual change that in many ways led to the new criteria. For example, previously, we could not be sure if a person identified with very mild dementia/MCI might be cognitively impaired due to underlying AD or due to a cause such as another dementing disorder (strokes or Lewy body dementia) or perhaps depression. With the new criteria, if the AD biomarkers are positive, one can then say with much more assurance that the person’s MCI or dementia is due to AD as opposed to another cause. Importantly, one can determine if AD biomarkers are present in people who are still cognitively normal. If the biomarkers are present, studies have shown that, depending on the specific biomarker being measured, the risk of becoming cognitively impaired due to AD is markedly increased.
Since no treatment for AD currently slows the progression or delays the disease and the FDA approved medications can only modestly improve the symptoms, assessment of biomarkers in cognitively normal people is still only recommended as part of a research study. However, biomarker research has important implications for the future. With substantial nerve cell death and synapse loss having already occurred at the clinical stage of very mild dementia/MCI, we will almost certainly need to treat people who are cognitively normal to try to delay the onset of cognitive decline. Further, to identify patients at high risk for cognitive decline, the use of biomarkers will be essential to confirm that they have “preclinical” AD—that is, the presence of AD pathology in the absence of symptoms and signs of dementia.
Development of future treatments for AD and the new criteria
Many promising disease-modifying treatments are in development, and some are already in human trials for patients diagnosed with AD. While trials of promising medications that could treat people with preclinical disease have not yet started, some are very likely to begin over the next year or two, involving people at very high risk of cognitive decline because they have a rare gene mutation that causes AD at extremely young ages (30-60). Also being discussed are future trials for cognitively normal people in the range of 60 to 90 years old, screening them for biomarkers and then enrolling only those at high risk for cognitive decline. The new focus on preclinical AD is not because new treatments cannot be developed for patients with either very mild dementia/MCI or dementia due to AD. Even in these circumstances, the use of biomarkers is important to be sure that the people being enrolled in clinical trials actually have AD and not another cause for their dementia and is now being incorporated by many pharmaceutical companies and academic groups in their quest to develop new treatments.
Summary
The new criteria for different stages of individuals with underlying AD pathology, including preclinical, MCI, and dementia, opens a new chapter in the annals of a long, very determined scientific effort. Twenty-seven years ago, four aspects of the science underlying this chronic disease were not yet clear, namely that: 1) there is a long preclinical period when AD pathology and brain damage are developing; 2) some people with MCI and dementia have cognitive decline due to underlying AD and some have other causes; 3) biomarkers can aid in the diagnosis of the different stages of AD; and 4) to ultimately develop the most effective therapies to delay or prevent cognitive decline and dementia, preclinical AD will need to be a target for future clinical trials. The new criteria will evolve as additional information is gathered, bringing us steadily closer to having effective treatments for one of the most important diseases in our society.
CONTENT PROVIDED BY
The Dana Foundation is a private philanthropic organization that supports brain research through grants and educates the public about the successes and potential of brain research.
Also In Archives
Trending
Popular articles on BrainFacts.org