A Burst from the Blue — Is Bulimia Nervosa Really a Modern Disease?
- Published20 Feb 2012
- Reviewed20 Feb 2012
- Source Wellcome Trust
Named in a scientific paper for the first time in 1979, bulimia nervosa has been studied extensively since. But while researchers explore its causes, diagnosis and treatment, the origins of the condition have attracted considerably less attention. Chrissie Giles meets two researchers who were instrumental in establishing bulimia nervosa as an eating disorder to find out more about their thoughts on its history.
Hearing voices in schizophrenia, hand washing in obsessive-compulsive disorder, and bingeing and vomiting in bulimia nervosa: in the public imagination, particular symptoms of some psychiatric conditions have almost come to represent the conditions themselves, even if not all patients experience them.
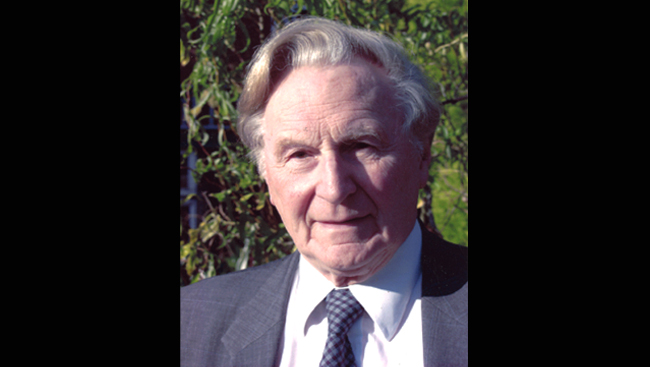
Emeritus Professor of Psychiatry at the Institute of Psychiatry and now a visiting Consultant Psychiatrist at The Priory Hospital, Hayes Grove, psychiatrist Gerald Russell published the first scientific paper naming bulimia nervosa (1). When he began working with patients with the condition, however, the bingeing aspect of the disorder initially eluded him. "If I tell colleagues or students now that I knew the patients were vomiting, but I didn't know that they were bingeing beforehand, they don't believe me," he says. "They say I must have been very blind - or stupid - not to have seen that."
It was 1972 when he first noticed a patient who was referred to the Royal Free Hospital for anorexia nervosa but didn't seem to fit the diagnostic criteria for the condition. He didn't know it then, but he had just seen the first of many patients suffering from bulimia nervosa, a disorder he went on to name in a paper published seven years later.
But was this really a new condition? If so, where did it come from, and why then? How has Gerald's original paper stood the test of what we've learned over the past three decades?
Between 1972 and 1977, Gerald saw 30 patients who didn't seem to fit their diagnoses of anorexia nervosa. In spite of persistent vomiting, most of these patients were of normal or near-normal weight - in contrast to the extreme underweight seen in those with anorexia nervosa. In some cases, menstruation continued - something rarely seen in women with anorexia nervosa.
"I knew this was a very difficult problem," says Gerald, who was attempting to treat the patients with the refeeding and nursing programmes used for anorexia nervosa. "I would present these cases at conferences as I wanted advice on how to treat them. They vomited or took laxatives, and they failed to respond to the ordinary measures for anorexia nervosa."
In the course of trying to help these "atypical, difficult, anorexic patients", he experienced what he describes as a small miracle. "In 1975, I had a patient who was very much in need of help. She happened to be a medical doctor and, coming to see the professor, she was on her best behaviour and she wanted to be very frank and very honest," Gerald says.
"She said something to me which led me to a sudden clarification, an epiphany. Simply: 'You should know that the reason I vomit is simply to get rid of all this food I eat.' 'Curious', I thought, and wrote it down, including details of the huge quantities of food she would ingest. I had not thought of that."
Armed with this information from patient 13 or 14 of the 30 he would eventually write about, he went back over some of the earlier cases and saw that they had also been overeating. "I changed the criteria from vomiting or laxative use to these behaviours plus overeating."
Naming names
He published his series of patients in a 1979 'Psychological Medicine' paper,1 the first time that bulimia nervosa had been identified and named. This group personified what he considered to be the key features of the condition: an irresistible urge to overeat followed by self-induced vomiting or purging, and a morbid fear of getting fat. Described by Gerald as "an ominous variant of anorexia nervosa", bulimia nervosa is now widely recognised as one of three main types of eating disorder.
Gerald Russell was not the only psychiatrist noticing patients with a different kind of eating disorder. Chris Fairburn, now a Wellcome Trust Principal Research Fellow and Professor of Psychiatry at University of Oxford, was a young doctor undertaking psychiatry training at the University of Edinburgh. In 1976, he had an experience similar to Gerald's. Asked to assess a patient referred by her GP for help with anorexia nervosa, Chris found himself face-to-face with someone who looked completely normal.
The patient was dieting, vomiting, exercising and taking laxatives, but her weight was normal - how could this be? In the pre-Google world of 1976, Chris went to the library to investigate, but in vain. "I tried to read the world literature on this, but there wasn't one," he says.
After several more appointments, he decided to ask the patient directly why her weight was normal. "With considerable embarrassment, she told me that she kept losing control over eating and was having repeated episodes of extreme overeating. She was very ashamed of this. She'd been very open in general, but she hadn't told me about this part. Her weight now made sense."
Gerald's and Chris's work on bulimia nervosa forms part of more than three decades of research into the condition, which is now well recognised across the world. It is listed in the World Health Organization's 'International Classification of Diseases' (ICD-10) and the American Psychiatric Association's 'Diagnostic and Statistical Manual of Mental Disorders' (DSM-IV), two key reference documents for different conditions.
Modern history?
Yet while conferences are full of sessions and journals replete with articles on how to diagnose, classify and treat bulimia nervosa, Gerald is puzzled by professional audiences' "relative indifference" to questions about the origins of the disorder.
Framed eloquently in 1990 by Dr Albert Stunkard, a psychiatrist at the University of Pennsylvania, one idea is that bulimia just appeared in the late 1960s: "Unlike anorexia nervosa, for which a rich history has been traced to the Middle Ages, bulimia nervosa seems to have burst from the blue upon modern society and it has achieved widespread recognition in a very short period of time." (2)
In an invited article in 'European Eating Disorders Review', coinciding with the 25-year anniversary of his seminal paper naming the condition, Gerald examined the evidence that bulimia nervosa is a new disorder (3). He cites three sources for this evidence: literature sources, retrospective diagnoses from clinical archives and cohort studies.
Looking through the pre-1950s psychiatric and medical literature, researchers have found classical cases that meet the diagnostic criteria set out by Gerald in 1979, but they also feature some important differences.
These classical cases include that of 'Patient D', a woman in her mid-20s. She was seen by the psychoanalyst Mosche Wulff in Berlin, who published details of the case in 1932. Patient D, like two other historical cases ('Nadia', described by Pierre Janet in 1903 and Ellen West, described by Ludwig Binswanger in 1944-45), satisfied the basic diagnostic criteria for bulimia nervosa - episodic overeating, compensatory vomiting, fasting and/or laxative use, and a dread of getting fat.
They were not straightforward cases, though. "They were usually unfortunate people who suffered from even more serious, severe and complicated symptoms - they had other problems, as well as the eating disorder," says Gerald.
Researchers have also trawled clinical archives to try to find descriptions of cases that would be considered as bulimia nervosa today. The archives of the Mayo Clinic, which contains data for the population of the city Rochester, Minnesota in the USA, are a rich repository of clinical information on all kinds of disease. Dr Alexander Lucas and colleagues from the Mayo Clinic studied these archives (4). "They looked at the case notes back as far back as they could - around ten years before bulimia nervosa was described - and could find only very atypical cases," Gerald says.
The third strand of evidence Gerald puts forward for bulimia nervosa being a new disorder is cohort studies. In these studies, the frequency of the illness is recorded in subjects grouped according to their dates of birth. The aim was to detect whether groups with more recent dates of birth were at higher risk of developing bulimia nervosa. He reports on three such cohort studies.
One concerned people on a twin register in the USA. Kenneth Kendler and colleagues looked at the prevalence of bulimia nervosa in three groups of subjects: those born before 1950, those born between 1950 and 1959, and those born after 1959 (5). The last groups - with the most recent dates of birth - had the highest prevalence of bulimia nervosa.
Other researchers have repeated this work, looking at women born during the same date intervals (6). They found the age of onset of bulimia nervosa to be younger in groups born in 1950 to 1959 and after 1959.
"This work suggested that whatever it was that made bulimia nervosa more common affected these young women around a crucial time when they were between 18 and 30, and this coincided with the 1960s," says Gerald.
Chris Fairburn's work showed similar findings. In the early 1980s, he and colleagues conducted the 'Cosmopolitan study' and the 'BBC study', named after the magazine and TV channel, respectively, through which people potentially suffering from bulimia nervosa were found (7,8). Through these studies, researchers identified large numbers of undetected cases in the 1980s. However, in no patients was the condition present before the late 1960s.
Cultural influence
So, did society cause bulimia nervosa to come into existence? "It was 'Twiggy' time," says Chris Fairburn, referring to Lesley Lawson, a thin, androgynous-looking model who came to prominence in the UK in the 1960s. "There's some evidence that the desired shape for women went down at this time, in terms of becoming lighter," says Chris, "and quite a few prominent women's magazines were publicising self-induced vomiting as a means of weight control. The theory is that widespread publicity about vomiting as a means of weight control triggered a new cohort of vulnerable young women into developing an eating disorder."
Does he put any stock in the modern refrain that women's magazines are behind many of the eating disorder cases seen today? "Very little," he says. "In the 60s and early 70s, it was unhelpful publicising self-induced vomiting as a means of weight control, but now everyone knows about this - even though it is ineffective.
"As for magazines being the cause of eating disorders, this doesn't hold water at all. After all, most young women in our society are exposed to cultural pressures to be slim, yet only a minority develop an eating disorder." He adds that there are a variety of established risk factors for developing an eating disorder, including ones likely to have a genetic basis.
Gerald thinks that bulimia nervosa reflects what society has become, and sees the societal influence as the "most economical explanation" for several reasons. "Partly, it's because the idealisation of a slender female figure is seen in the fashion industry and in magazines, and coincides with the preoccupations of schoolgirls.
"Also important is the realisation that comes from talking to patients that they use the same language - that was a surprise to me when I was a beginner." He recounts a conversation with a patient where he found himself negotiating what weight she would go to, rather simply telling her his plan. "My professor, Aubrey Lewis, was furious with me. My patient produced objections to me telling her to put on weight and my professor reprimanded me for getting into that argument. I think he was partly right." Such experiences underlined for him the extent and influence of patients' "dread of fatness".
Classifying and categorising
As would be expected, during the decades since bulimia nervosa was first recognised, the way healthcare professionals talk about and classify it has changed. All across psychiatry, classification is popular - "a sort of contagious influence", says Gerald.
"The classification of psychiatric illness is everybody's bee in their bonnet, and I can see why: I get interested in spite of myself," he says. "The reason it is interesting is that the great hope is to have one label for an illness that you can recognise, so that treatment will follow automatically. That's pie in the sky, unfortunately."
He sees the value in classifications like 'Diagnostic and Statistical Manual of Mental Disorders', which takes blocks of symptoms and, by calling them syndromes, provides a useful language for clinicians. "But if you're more ambitious about classification and say that a particular label means that this condition is a 'disease entity', with specific causes and a specific treatment, that's overoptimistic, like gazing into a crystal ball," he says.
Chris Fairburn is less convinced about the value of the current diagnostic distinctions. He points out that they lead clinicians to neglect two properties of eating disorders: that these disorders share most of their core clinical features, and that most patients move between various eating disorder diagnoses. With support from the Wellcome Trust, he has developed a single psychological treatment for all eating disorders, which is designed to target the causal processes that maintain their core features (9). The results from his group and others show that the treatment is effective and 'transdiagnostic': a patient's diagnosis has no bearing on their outcome.
Writing his now-famous 1979 paper, Gerald recognised the overlap between eating disorders, describing bulimia as a new entity, but a variant of anorexia, "so they're separate but overlap," he says.
What was it about his experiences that made him pick "ominous" as the term to describe the disorder? "I saw bulimia nervosa as a later stage of anorexia nervosa, as unrecovered anorexia. I thought, here's somebody getting stuck in bulimia nervosa and that they might not recover." He also explains that this reflected the fact that he saw the most difficult patients (adding, with a smile, that every eating disorder specialist claims this). In some patients, he noted disturbances in blood electrolytes (which can result from frequent purging), as well as serious mental disturbance. Several patients died during the study, at least one from suicide.
"I had the idea that probably the course [of bulimia nervosa] would be a long one and these patients were more in danger than those with anorexia nervosa. But on the whole, today, I would accept that the outcome is better than in anorexia nervosa," he says. "Now, I would say that 'ominous' is incorrect."
CONTENT PROVIDED BY
Wellcome Trust
References
1 Russell GFM. Bulimia nervosa: an ominous variant of anorexia nervosa. Psychol Med 1979;9:429-448.
2 Stunkard A. A description of eating disorders in 1932. Am J Psychiatry 1990;147:263-8.
3 Russell GFM. Thoughts on the 25th anniversary of bulimia nervosa. Eur Eat Disorders Rev 2004;12:139-152.4 Lucas AR and Soundy TJ. The rise of bulimia nervosa. Ninth World Congress of Psychiatry, Rio de Janeiro, Brazil, June 6-12 1993, Abstract 544, p.139.
5 Kendler KS at el. The genetic epidemiology of bulimia nervosa. Am J Psychiatry 1991;148(12):1627-37.
6 Garfinkel PE et al. Bulimia nervosa in a Canadian community sample: prevalence and comparison of subgroups. Am J Psychiatry 1995;152(7):1052-8.
7 Fairburn CG and Cooper PJ. Self-induced vomiting and bulimia nervosa: an undetected problem. Br Med J (Clin Res Ed) 1982;284(6323):1153-5.
8 Fairburn CG and Cooper PJ. Binge-eating, self-induced vomiting and laxative abuse: a community study. Psychol Med 1984;14(2):401-10.
9 Fairburn CG et al. Transdiagnostic cognitive behavioral therapy for patients with eating disorders: a two-site trial with 60-week follow-up. Am J Psychiatry 2009;166:311-9.Also In Archives
Trending
Popular articles on BrainFacts.org