Is the Brain Really Sterile? Fish Study Reignites Controversy
- Published23 Oct 2025
- Author Sophie Fessl
- Source BrainFacts/SfN

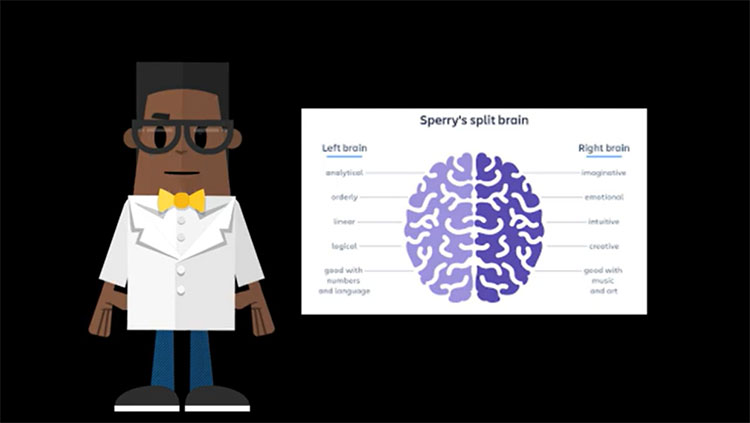
The human body is teeming with microbes. Bacteria, fungi, and even viruses play a key role in maintaining our overall health. The stomach, skin, and other parts of the body require a thriving microbiome to function properly. But unlike other organs, the brain has traditionally been considered germ free. Most neuroscientists will tell you the wall of cells protecting it, called the blood-brain barrier, ensures it remains sterile.
For the past decade, however, this conventional wisdom has been up for debate. Experts in the field argue about whether bacteria could live in human brains — healthy or otherwise — and, if so, what effect they have there. Some researchers insist bacteria basically can’t get into the brain at all, with highly limited exceptions to this rule. Others think bacteria slip into the brain later in life, when its barrier begins to weaken. And still, others contend that bacteria are always there, just in small numbers, but become more abundant as we age.
In 2024, a group of researchers published their findings after culturing bacteria from the brains of fish, issuing a new challenge in favor of the idea that microbes can indeed be identified within animal brains. Amid the ongoing conversation over whether the brain has a true microbiome, these results could have major implications for how we understand the brain’s relationship to bacteria and brain health more generally — or, they could turn out to be a major scientific mix-up.
Analyzing the Catch of the Day
University of New Mexico immunologist Irene Salinas didn’t expect to find bacteria in fish brains — she was initially studying nasal immunity.
Salinas suspected microbes from the nose could enter the olfactory bulb, the brain structure most closely connected to the outside environment. Within vertebrates, it’s responsible for sending smell information from the nose to the brain. Her goal was to assess whether olfactory bulbs sampled from lab-raised trout have a microbiome modulating their immune system.
Salinas asked a student in her lab to sample other parts of the fish brains to act as controls, because she expected the olfactory bulb would contain far more bacteria compared to other, deeper brain regions. But the results were a surprise.
“We kept finding bacteria in every area of the brain,” Salinas said. “Actually, the olfactory bulb was the brain region with the lowest number of bacteria.”
The finding prompted Salinas and her team to look closer. In a 2024 study, they took samples from four fish brain regions — the olfactory bulb, telencephalon, optic tectum and cerebellum — and put them on plates researchers use to grow bacteria. They ended up culturing 54 species. And it’s not just an oddity of trout. When Salinas repeated the experiment using wild Chinook salmon samples, bacteria once again thrived.
Salinas knew her findings would face pushback. Neuroscientists have hotly debated the question of whether bacteria can live in the brain since 2013, when a group of researchers analyzed brain samples from people living with HIV. They identified RNA-based genetic signatures of bacteria and of viruses that attack bacteria, called bacteriophages. They also spotted these signatures in the HIV-negative control samples, suggesting healthy brains harbored bacteria, too.
Since then, other researchers have stumbled upon additional signs of microbial life in human and animal brains. One 2023 study, which was published as a preprint and has yet to be peer reviewed, found genetic signatures of bacteria and fungi in the brains of Alzheimer’s patients. Those researchers also identified signatures in healthy human brains and in animals including fruit flies, octopuses, frogs, and chickens. In 2018 and 2019, another group found fungal structures in brain tissue from people with Alzheimer’s and Huntington’s disease, respectively.
But not all scientists are convinced bacteria can enter and live in the brain. When a different group of researchers looked for genetic signatures of bacteria in healthy brains and in those of people with Parkinson’s disease, they didn’t find any. Genetic signatures they initially identified as bacterial turned out to either be contamination from the environment or errant human DNA.
Is it Real — or Just Noise?
The question of contamination is a major dilemma: Because microbial traces are so sparse compared to the human or animal DNA present in any given sample, even tiny contaminants may create the impression that microbes live in the brain when, really, they don’t.
Contamination can come from various sources. Basic laboratory tools, including the water used to prepare samples, often contain bacterial DNA. The brain samples themselves can be difficult to fully isolate, too. Bacteria from blood vessels in and around the brain may make their way into sequence data, meaning the results don’t solely reflect the microbial composition of brain tissue.
Another facet of the debate centers on methods. Sequencing involves detecting only fragments of all DNA present in a sample. “You don’t know what’s alive and what’s dead,” said David Corry, a professor at the Baylor College of Medicine.
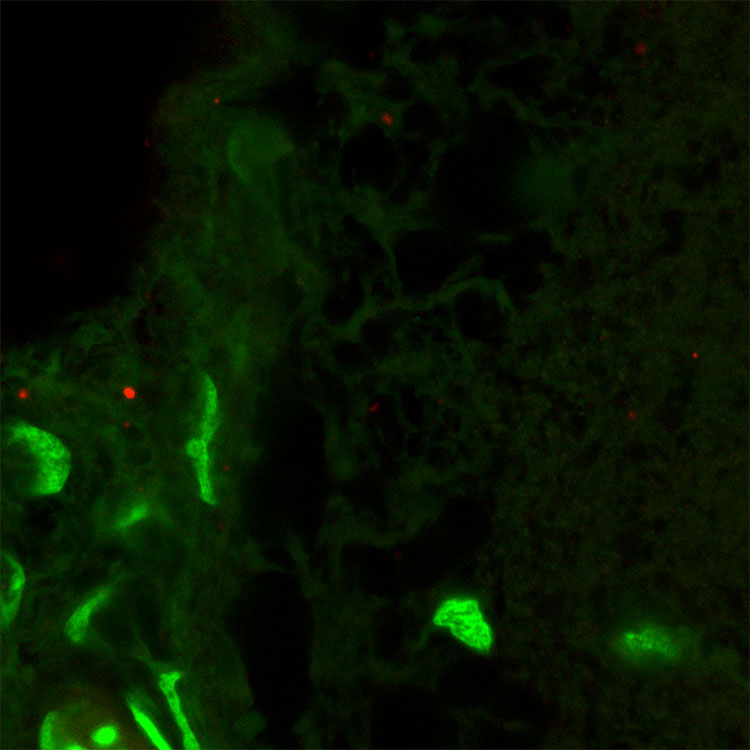
But Salinas’ team cultured live bacteria from their samples, which they concluded indicates the bacteria they identified weren’t dormant or dead, but truly living in the brain. “Not only are the microbes there, they are viable,” said Christopher Link, an associate professor of integrative physiology at the University of Colorado, Boulder, who wasn’t involved in the study. Looking under the microscope, Salinas noted she even spotted a bacterium caught in the middle of crossing the blood-brain barrier.
But getting her team’s paper through peer review wasn’t easy, Salinas said, and reviewers asked for “endless” measures to ensure their samples weren’t contaminated with bacteria from the lab or other parts of the fish. Her team sterilized the fishes’ exterior, tested lab materials and surfaces for contamination, and compared microbes from other organs and water samples.
“This gave us the peace of mind that we recovered what was really in the fish brain,” Salinas said.
Some critics argue bacteria can only slip into the brain after death, when the blood-brain barrier breaks down. But Salinas and her team took steps to prevent this. They drained blood from the fishes’ brains before euthanasia, and only then removed the tissue. She said this approach ensured any bacteria they found truly originated in the brain, rather than the capillaries weaving through it.
Link believes Salinas’ conclusions hold up to scrutiny. For him, one key aspect of Salinas’ experiment clinched the case. She and her colleagues added fluorescent bacteria to the fish tanks. Later, they found those same bacteria in the fish’s brains. “There is no other explanation — the bacteria got into the brain,” he said.
Neurodegenerative Diseases: Is a Rethink Needed?
Findings so far in humans and in animals may not necessarily prove the existence of a true microbiome in the brain. Unlike in the gut, where bacteria are plentiful and directly tied to its health, any microbes discovered in the brain may instead be accidental trespassers or sparse occupants. “I believe in the potential that our brains may be under a constant, low-level of intrusion of microbes,” Link said. “The evidence certainly does not support a microbiome in the sense of the gut microbiome.”
Clarifying our understanding of the brain’s relationship to bacteria could reshape how we understand neurodegenerative diseases. For example, researchers currently believe Alzheimer’s arises when a sticky protein called amyloid beta clogs up the brain. Some think this protein is intended to act as an antimicrobial agent. “Amyloid beta and alpha synuclein — the protein in Parkinson’s disease — all seem to be part of the brain’s immune response,” Corry said.
Corry’s perspective suggests neurodegenerative disease develops not from a single cause but from multiple attacks on the brain, one of which may be bacterial infection. With age, the blood‑brain barrier gets leakier, and the brain becomes less efficient at clearing microbes. More bacteria may enter the brain, potentially triggering its secondary immune response, leading to toxic protein accumulation and, ultimately, neurodegeneration. Salinas said the aging Chinook salmon her team studied showed signs of both amyloid-beta deposition and higher bacterial loads in their brains.
“Things can get into the brain — how much and whether it matters is the question.” — Christopher Link
However, the debate is far from settled, but it does challenge current thinking about the brain. “What’s certainly true is that the blood-brain barrier isn’t perfect,” Link said. “Things can get into the brain — how much and whether it matters is the question.”
CONTENT PROVIDED BY
BrainFacts/SfN
References
Alonso, R., Pisa, D., Fernández-Fernández, A. M., & Carrasco, L. (2018). Infection of fungi and bacteria in brain tissue from elderly persons and patients with Alzheimer’s disease. Frontiers in Aging Neuroscience, 10, 159. https://doi.org/10.3389/fnagi.2018.00159
Alonso, R., Pisa, D., & Carrasco, L. (2019). Brain microbiota in Huntington’s disease patients. Frontiers in Microbiology, 10, 2622. https://doi.org/10.3389/fmicb.2019.02622
Bedarf, J. R., Beraza, N., Khazneh, H., et al. (2021). Much ado about nothing? Off-target amplification can lead to false-positive bacterial brain microbiome detection in healthy and Parkinson’s disease individuals. Microbiome, 9, 75. https://doi.org/10.1186/s40168-021-01012-1
Branton, W. G., Ellestad, K. K., Maingat, F., Wheatley, B. M., Rud, E., … Power, C. (2013). Brain microbial populations in HIV/AIDS: α-Proteobacteria predominate independent of host immune status. PLOS ONE, 8(1), e54673. https://doi.org/10.1371/journal.pone.0054673
Hu, X., McKenzie, C. A., Smith, C., Haas, J. G., & Lathe, R. (2023). [Preprint]. bioRxiv. https://doi.org/10.1101/2023.02.06.527297
Kandalai, S., Li, H., Zhang, N., Peng, H., & Zheng, Q. (2023). The human microbiome and cancer: A diagnostic and therapeutic perspective. Cancer Biology & Therapy, 24(1), 2240084. https://doi.org/10.1080/15384047.2023.2240084
Link, C. D. (2021). Is there a brain microbiome? Neuroscience Insights, 16, 1–5. https://doi.org/10.1177/26331055211018709
Maldonado, T. A., Jones, R. E., & Norris, D. O. (2000). Distribution of β-amyloid and amyloid precursor protein in the brain of spawning (senescent) salmon: A natural, brain-aging model. Brain Research, 858(2), 237–251. https://doi.org/10.1016/S0006-8993(99)02328-8
Mani, A., Henn, C., Couch, C., Patel, S., Lieke, T., Chan, J. T. H., Korytar, T., & Salinas, I. (2024). A brain microbiome in salmonids at homeostasis. Science Advances, 10(38), eado0277. https://doi.org/10.1126/sciadv.ado0277
Rieder, R., Wisniewski, P. J., Alderman, B. L., & Campbell, S. C. (2017). Microbes and mental health: A review. Brain, Behavior, and Immunity, 66, 9–17. https://doi.org/10.1016/j.bbi.2017.01.016
Tan, A. H., Lim, S. Y., & Lang, A. E. (2022). The microbiome–gut–brain axis in Parkinson disease—from basic research to the clinic. Nature Reviews Neurology, 18, 476–495. https://doi.org/10.1038/s41582-022-00681-2
Also In Anatomy
Trending
Popular articles on BrainFacts.org