Mitigating the Opioid Crisis
- Published2 Nov 2018
- Reviewed2 Nov 2018
- Authors Stephani Sutherland, Marissa Fessenden
- Source BrainFacts/SfN

For millennia, humans have employed opium and its derivatives to quell pain. Ancient societies including Rome, Greece, Mesopotamia, Egypt, and Asia, all cultivated opium poppies. To this day, opioids excel at tamping down the acute pain associated with surgery or severe injury.
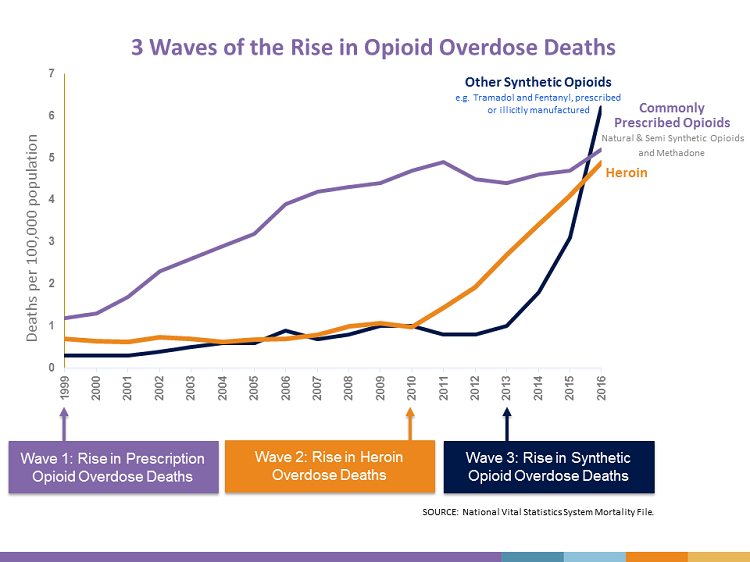
For people suffering daily chronic pain, as an estimated 25 million Americans and 20 percent of people worldwide do, opioids may be ineffective while at the same time causing serious — even deadly — side effects. Unfortunately, the open-ended use of opioids to treat chronic pain — particularly in the US — has fueled an opioid addiction epidemic.
In response to this rising epidemic, neuroscience researchers from around the world are working to develop new treatments for chronic pain.
“Tens of thousands of people who take opioids die every year, and so we need safer and more effective drugs for treating pain and related conditions,” said Bryan Roth, Michael Hooker Distinguished Professor at the University of North Carolina School of Medicine.
Opioids quell pain by mimicking endorphins — neurotransmitters that bind opioid receptors in the brain and relieve pain. But, side effects like respiratory depression, what kills people who overdose, and dependence, tolerance, and addiction — three separate but intertwined physiological effects — limit the use of opioids.
After one week of regular opioid use, all patients become dependent — they experience physical withdrawal including nausea and increased pain sensitivity if they stop taking the drug. Tolerance develops with longer-term use — the opioid dose that once relieved pain becomes inadequate, and the patient requires a higher dose. Addiction, or substance use disorder, is more complicated. People addicted to drugs seek the euphoric “high” that opioids produce and take them inappropriately, often at great risk including death by overdose. Interfering with the development of any of these side effects could help save lives.
Without question, opioids quiet pain, but they also trigger many side effects including constipation, nausea, anxiety, addiction, and respiratory depression. Roth’s group aimed to design pain-relieving drugs without side effects. Opioids relieve pain by acting at four different receptors, including the mu- and kappa-receptors, which were discovered in the 1970s. Activating mu opioid receptors relieves pain but risks addiction and respiratory depression. Drugs aimed at the kappa opioid receptor also relieve pain but cause hallucinations.

Roth’s team reasoned that knowing the structure of an activated receptor could guide their efforts. His team focused on solving the structure of the kappa opioid receptor (KOR). Using nanoantibodies to stabilize the receptors, the researchers mapped the structure of the activated KOR and synthesized a compound to fit snugly into it. The compound activated the pathway lessening pain without triggering the pathway leading to respiratory depression and dependence. Roth’s team and others are using these structures to discover new medicines in a systematic way. “Now that we have the structures, we can actually discover these medications or these medicine-like compounds in a systematically schematic way,” Roth said.
Taking a different tack, Japanese research focused on tolerance. A team led by Taka-aki Koshimizu of Jichi Medical University and Yukio Takano of Fukuoka University identified a molecular complex — comprising vasopressin 1b receptors, mu-opioid receptors, and beta-arrestin-2 — that not only heightens pain, it also accelerates morphine tolerance. Working with mice, the researchers disrupted the complex, slowing the development of tolerance without increasing pain. Drugs that break up this complex may reduce the amount of an opioid needed to treat pain by preventing tolerance.
For people dependent on opioids, stopping the drug outright means undergoing the muscle aches, nausea and vomiting, and diarrhea associated with opioid withdrawal. People are so driven to avoid these unpleasant side effects that they present an enormous hurdle to quitting. Tuan Trang, a researcher at the University of Calgary, and his team explored the underlying causes of opioid withdrawal.
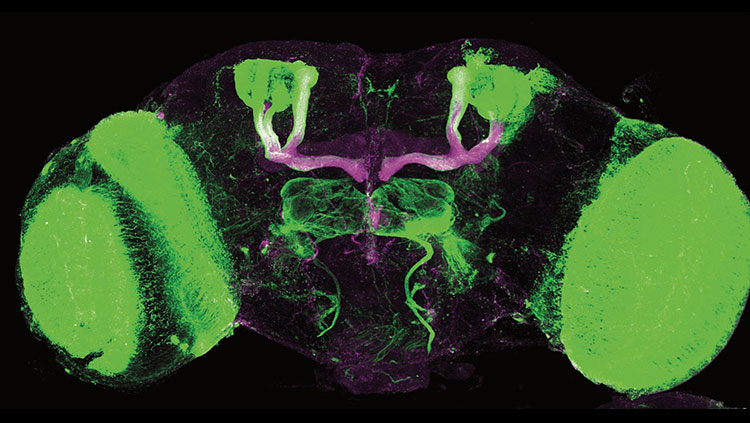
His team focused on microglia, specialized immune cells in the brain and spinal cord thought to be associated with opioid withdrawal. Working with mice and rats, the researchers blocked the pannexin-1 channel on microglia, alleviating the animals’ withdrawal symptoms. They also discovered that an anti-gout medicine called probenecid could block these channels, without affecting pain relief. Trang and his team are working to develop a clinical trial to test probenecid in humans.
The opioid crisis “must be addressed in a comprehensive, integrated, and strategic fashion,” says Nora Volkow, director of the National Institute on Drug Abuse (NIDA), because it arises from interrelated factors including mismanagement of chronic pain, the availability of opioids, and economic distress.
NIH in collaboration with the FDA and the private sector is working to accelerate biomedical research focused on stemming the opioid crisis by improving treatments for opioid misuse disorder and addiction, and by finding new treatments for chronic pain. Launched in April 2018, the program is called the Helping to End Addiction Long-term (HEAL) Initiative.
That funding will boost efforts to find new non-addictive pain medications, such as those targeting voltage-gated sodium channels. Sodium channels provide the spark that helps neurons to “fire,” and blocking them would short-circuit pain signals from reaching the spinal cord.
“When you sit in the dentist’s chair, you don’t feel pain, because they have blocked your sodium channels with anesthetic,” said Sulayman Dib-Hajj of Yale School of Medicine and the Veterans’ Affairs Medical Center. “The problem is the drugs are not selective.” Sodium channels are key to running the heart and brain as well as peripheral nerves, so blocking them all would be deadly.
One attractive drug target came from the realization in the 1990s that a particular channel called Nav1.7 is found only in peripheral nerves. Theoretically, a drug could block Nav1.7 and pain without stopping the heart and brain. The discovery that inherited pain syndromes result solely from genetic mutations in the gene for Nav1.7 solidified its potential as a target, and about a half dozen companies are currently developing drugs aimed at Nav1.7.
Another strategy employs the use of antibodies, tiny peptides aimed at proteins that contribute to pain sensations. Recently, the U.S. Food and Drug Administration approved an antibody aimed at the calcitonin gene-related peptide, a protein that causes migraine headaches. Nerve growth factor (NGF) is another pain associated protein. It stimulates the growth and differentiation of neurons. It also serves as a pro-inflammatory mediator at pain sensing neurons. Antibodies blocking NGF should dull pain. Early clinical studies of anti-NGF antibodies caused joint damage in some osteoarthritis patients. Researchers improved the safety of the treatment and more trials are now underway.
A concerted effort on the part of scientists and health care providers is important to overcome this crisis because it “impacts all of us, not just [people addicted] to opioids,” Trang says.
CONTENT PROVIDED BY
BrainFacts/SfN
Discussion Questions
(1) What are the risks associated with using opioids to treat chronic pain?
(2) What are some of the opioid alternatives currently being investigated?
(3) Why is it important to develop alternative treatments for chronic pain?
Also In Addiction
Trending
Popular articles on BrainFacts.org