Neuroethics of Clinical Research and Treatment
- Published1 Apr 2012
- Reviewed1 Apr 2012
- Source BrainFacts/SfN
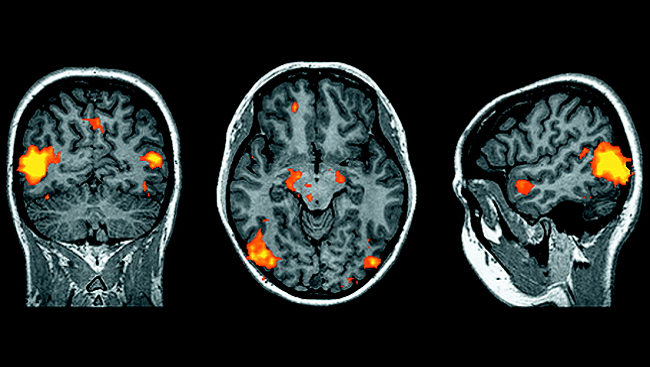
Neuroscience already has given rise to drugs and devices, developed for the treatment of illness, that permit healthy people to improve their cognitive performance or alter their emotional states. In the future, drugs may be developed that enhance memory or alter social behaviors.
It is critical that scientists engage policymakers and society at large in discussions about the extension of treatments from the realm of illness to the realm of enhancement. Neuroethical issues in medicine arise when gaps exist between diagnosis and treatment, treatments may offer tradeoffs in personality or cognitive changes, and drugs or devices that can help unwell patients also can boost performance of normal people.
For example, when diagnostic tests exist for brain-based diseases that have no cure, such as Alzheimer’s, how should the tests be used? Should emergency rooms administer memory-altering drugs to patients who have suffered a trauma and may be at risk for post-traumatic stress disorder? If drugs that are effective for treating attention deficit hyperactivity disorder also improve work or classroom performance of normal people, do we need to regulate access, and do we consider such use to be cheating? More questions of this type will emerge as our knowledge increases.
Informed Consent in Research
Special care must be taken when scientists seek consent to conduct human research and throughout experiments, especially when potential research subjects have thinking or emotional impairments that might affect their decision-making capacity. Consent is an ongoing process that should involve education of the potential research participant and, when appropriate, family members. Researchers are discussing potential needs to exercise greater scrutiny, ensure safeguards, and enhance participants’ grasp of a study, including risks and benefits.
CONTENT PROVIDED BY
BrainFacts/SfN
Also In Archives
Trending
Popular articles on BrainFacts.org