Looking Into Psychedelics for Alzheimer's Research
- Published13 Dec 2022
- Source BrainFacts/SfN
Psychedelic drugs have had a resurgence — but not in the way you might expect. Psychedelics such as LSD and psilocybin induce hallucinations that warp perception. But the drugs also have specific biological actions that could potentially treat mental health conditions and impact diseases affecting the brain, including Alzheimer’s disease. Lab studies suggest psychedelics may also improve memory, focus, and learning. And psychedelics may treat the depression that can come along with diseases like Alzheimer’s.
This is a video from the 2022 Brain Awareness Video Contest.
Created by Sofia Cruz.
CONTENT PROVIDED BY
BrainFacts/SfN
Transcript
Melting walls, breathing objects, surreal geometric patterns, and intensifications of color and sound. These effects being described are characteristic of a psychedelic experience or so-called "trip."
Psychedelics like LSD, psilocybin, and DMT are types of hallucinogenic drugs that can produce changes in perception, emotion, and thinking. Though drug laws in the 1960s to 80s nearly halted research on these fascinating substances, the dialing down of these controls has led to a rebound in psychedelic research in neuroscience. Much of this research is focused on the possibility that psychedelics could treat various mental disorders, one of them being Alzheimer's disease.
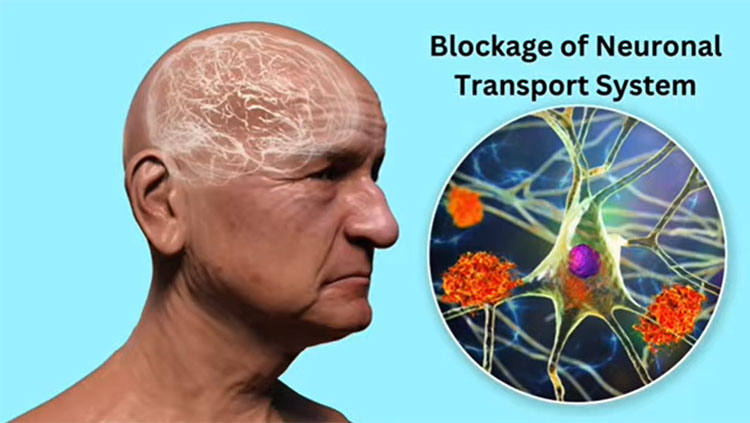
Alzheimer's disease is a brain disorder usually occurring in seniors that disrupts the communication between neurons and causes cell death, especially in regions involved in memory, attention, and learning. This interruption of signals is caused by the buildup of harmful proteins called neurofibrillary tangles and amyloid beta, which lead the brain to turn up its defense system and become inflamed.
Scientists suspect a way to ease this inflammation is by switching on a special receptor called the serotonin 2A receptor, which psychedelics have been shown to activate. In a healthy brain, there are high concentrations of the serotonin 2A receptors in regions most vulnerable to Alzheimer's, like the prefrontal cortex and the hippocampus. Activating the 2A receptors, particularly in these parts, could alleviate the brain inflammation, and resulting cognitive decline, that comes with the condition. In fact, recent studies on both rats and humans found that the activation of the 2A receptors using various psychedelics reduced brain inflammation, while memory, learning, and focus improved.
Moreover, scientists believe that activating this receptor with psychedelics can release chemical signals that help form new nerve cells and strengthen connections. This may help reverse the loss of cell function and death that occurs in Alzheimer's. A study on rats tested the effects of the psychedelic DMT on nerve tissue growth in the hippocampus linked to memory and learning.
In one experiment, researchers measured the time it took for a group dosed with DMT versus a group without DMT to find an escape platform in a water tank. As it turns out, the learning and recall performance of the DMT group was better. Another experiment presented the rats with two objects first. Then after a break, one of the objects was replaced with the new one. A rodent that remembers the old object usually spends more time exploring the new object. The DMT group spent a longer time examining the new object, demonstrating that the psychedelic boosted the memory capabilities of the rats.
Not only do psychedelics have the potential to advance cognitive performance in Alzheimer's patients, they may also help treat the depression and decrease in quality of life associated with the condition. Various studies at John Hopkins University have shown this, including one that dosed depressive cancer patients with LSD and psilocybin.
We know there is evidence suggesting that psychedelics could help treat Alzheimer's, but are there any risks that come with these substances? Psychedelics are actually nontoxic, safe, and are proven to not lead to a physical reliance or an addiction.
Also, though hallucinations from psychedelics are thought to cause fatal accidents, the risk is only significant when the drug is used in a recreational or uncontrolled setting. Despite the extensive research on how psychedelics could treat many brain disorders including Alzheimer's, there are some setbacks the field is facing, notably the placebo "unmasking" problem. Many psychedelic studies on humans are placebo-controlled trials in which one group of participants gets the actual drug being studied, while the other group gets a fake drug called a placebo.
Participants should not know whether they are receiving the real or placebo treatment, otherwise their expectancies of the drug's effects may cause them to report false outcomes. Yet, because it is difficult to recreate the immediate effects of actual psychedelics, many participants will likely guess correctly which group they are in. This may have caused some human studies to overestimate the benefits of psychedelics to cognitive ability and mental health. Though placebo "unmasking" cannot happen in animal studies since the subjects do not have prior expectations, there have been no psychedelic studies on animals that accurately model the mechanisms of Alzheimer's disease.
So, what exactly do we know so far? There is a good chance that psychedelics could be used to treat Alzheimer's, but much more work needs to be done. Scientists should continue to find new ways to sharpen the accuracy of their research, while remaining transparent in reporting their experiment conditions. Regardless of current limitations and challenges, the neuroscience community should not give up on this groundbreaking opportunity that could possibly improve many lives. After all, this field has just begun to take off.
Also In Alzheimer's & Dementia
Trending
Popular articles on BrainFacts.org